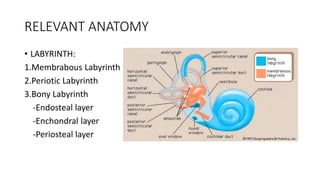
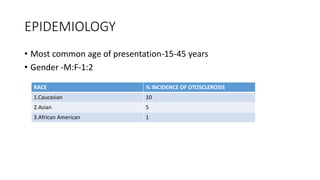
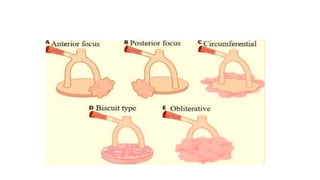
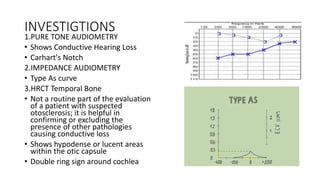
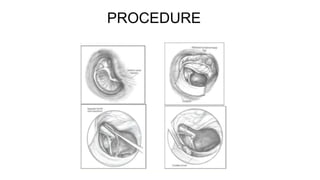
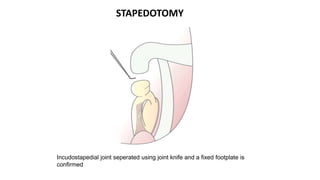
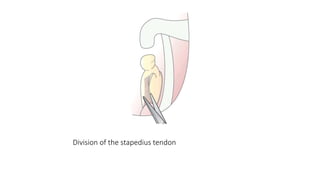
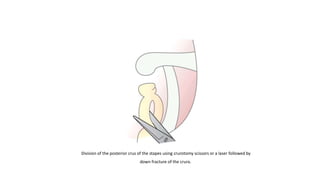
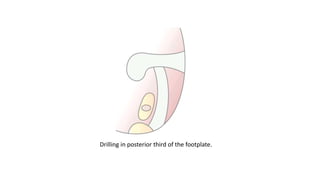
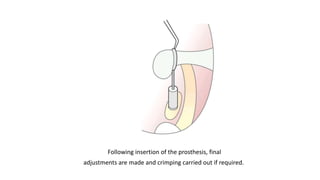
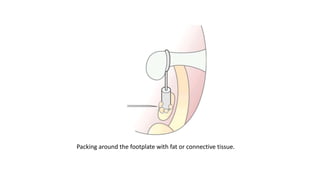
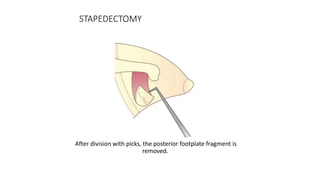
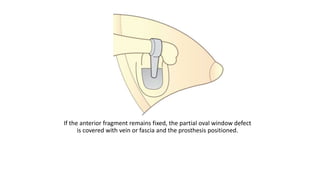
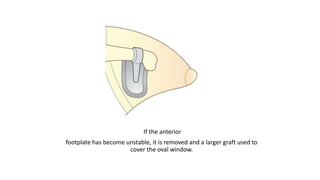
This document provides information on otosclerosis, including its definition as a hereditary disorder involving abnormal bone metabolism in the otic capsule. It discusses the relevant anatomy, etiology including genetic and viral factors, epidemiology with higher rates in Caucasians and females, pathogenesis through bone remodeling, clinical presentation of progressive hearing loss, investigations such as audiometry and CT scans, medical treatments including sodium fluoride and bisphosphonates, surgical treatments like stapedotomy and stapedectomy, complications, and procedures for these surgeries.