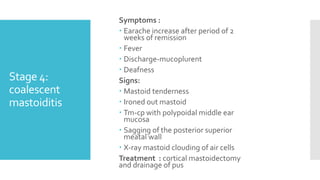
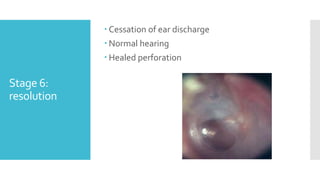
This document discusses otitis media with effusion (OME), also known as serous otitis media (SOM). It defines OME as a chronic accumulation of mucus within the middle ear, which can cause conductive hearing loss. It discusses the pathogenesis, etiology, symptoms, investigations and treatment of OME. It also discusses acute suppurative otitis media (ASOM) and chronic suppurative otitis media (CSOM), outlining their stages, complications, and surgical treatments including myringotomy and myringoplasty.
![SOM,ASOMANDCSOM [TTD]
PRINCIPALS OF MANAGEMENT
AND SURGICAL APPROACHES
SEMINAR PRESNTED BY
DRV SANKAR NAIK](https://image.slidesharecdn.com/3rdseminarvsn-221106050928-9d2956e4/85/3RD-SEMINAR-VSN-pptx-1-320.jpg)