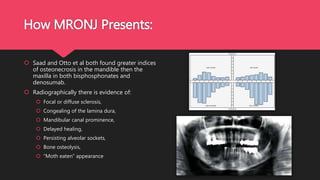
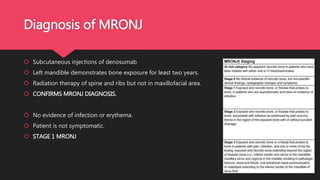
This document presents a case of a 70-year-old male diagnosed with medication-related osteonecrosis of the jaw (MRONJ) due to monthly denosumab injections for metastatic cancer since 2011. Clinical and radiographic findings were consistent with MRONJ including exposed bone in the area of teeth #34 and #36 that had been extracted in 2012. The patient's stage 1 MRONJ was managed conservatively with chlorhexidine rinses and referral for surgical debridement if infection develops. The document discusses denosumab versus bisphosphonates, diagnosing and staging MRONJ, potential pathophysiology, presentation, treatment guidelines, and recommendations for preventing MRONJ in patients taking anti-resor
![Medication Related Osteonecrosis of
the Jaw
[MRONJ]
Brendan Da Silva Proserpine Hospital](https://image.slidesharecdn.com/49ec120f-b97e-4162-9f98-f04f0c595f60-160731061729/85/MRONJ-PRESENTATION-1-320.jpg)





![Diagnosing MRONJ
Characteristics determined by the American Association of Oral and Maxillofacial Surgeons
[AAOMS] include:
1. Current or previous treatment with anti-resorptive or anti-angiogenic agents;
2. Exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial
region that has persisted for more than eight weeks;
3. No history of radiation therapy to the jaws or obvious metastatic disease to the jaws.](https://image.slidesharecdn.com/49ec120f-b97e-4162-9f98-f04f0c595f60-160731061729/85/MRONJ-PRESENTATION-7-320.jpg)