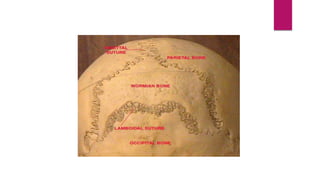
Osteogenesis imperfecta is a connective tissue disorder caused by mutations in the COL1A1 and COL1A2 genes, resulting in abnormal type 1 collagen. This leads to bones that are fragile and prone to fractures from minor trauma. Clinical features include recurrent fractures, bone deformity, blue sclera, dental abnormalities, and hearing loss. It is classified into four types based on severity, with type 1 being the mildest form. Diagnosis is based on clinical and radiological findings, and may include collagen or DNA analysis. Treatment focuses on physiotherapy, orthotics, bisphosphonates, and surgery to correct deformities and stabilize bones.