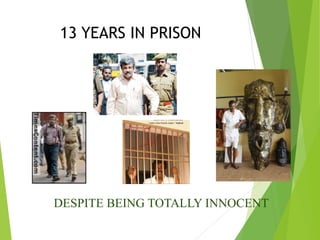
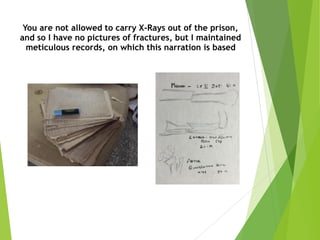
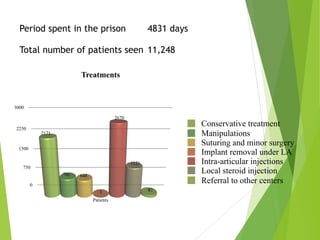
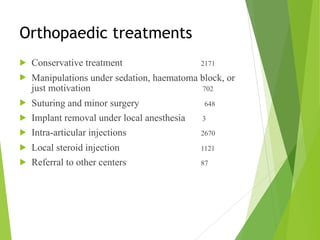
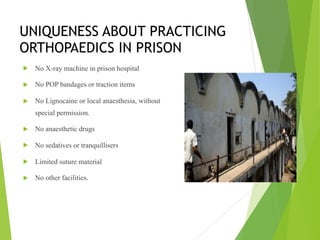
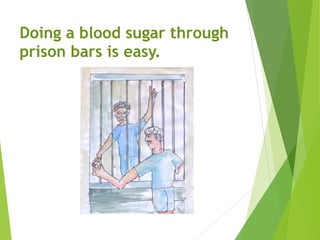
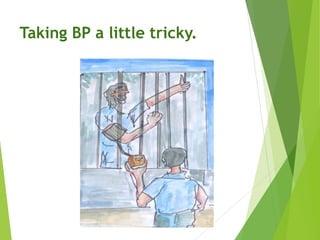
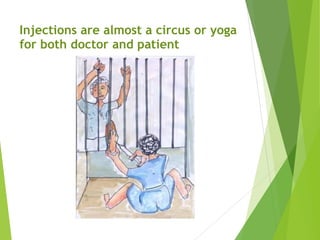
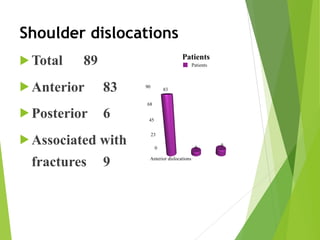
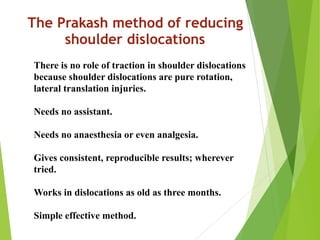
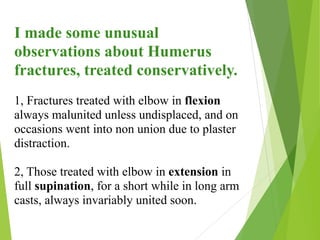
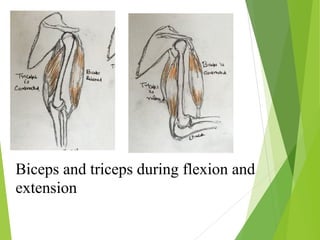
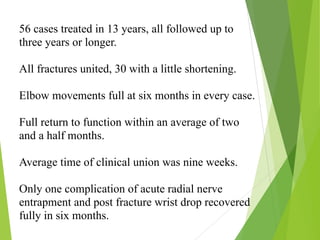
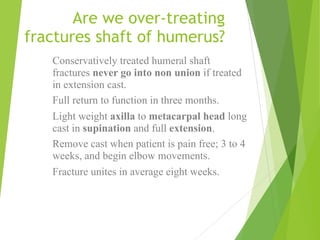
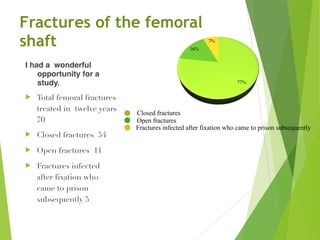
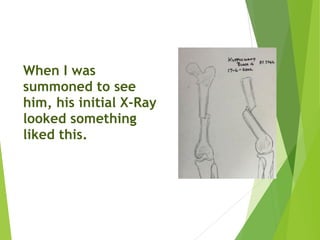
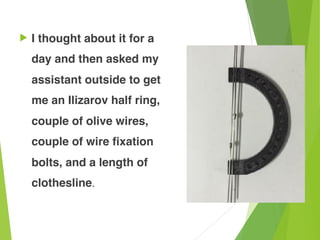
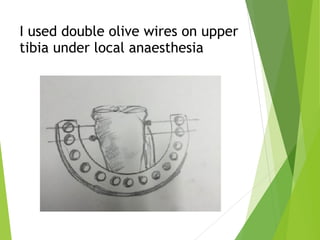
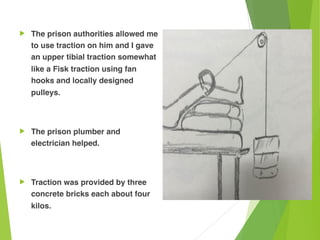
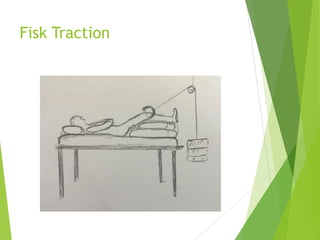
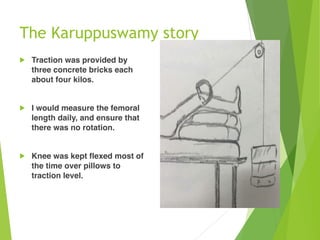
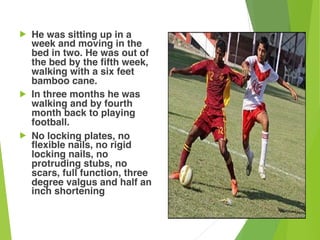
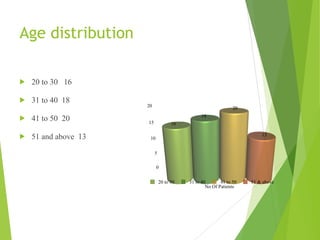
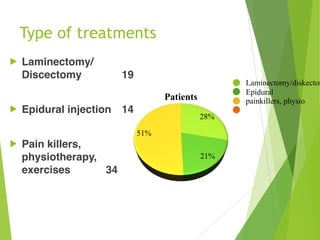
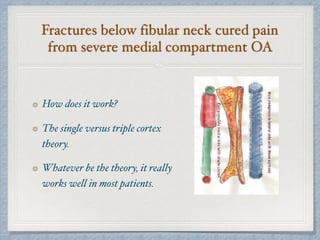
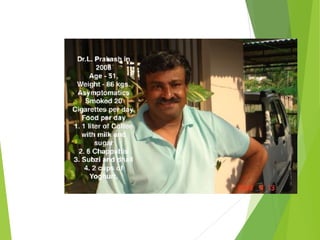
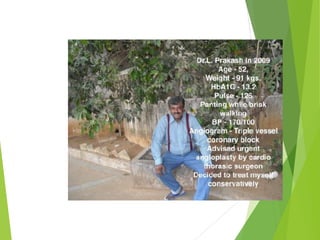
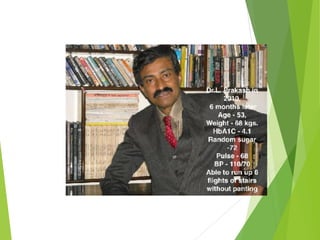
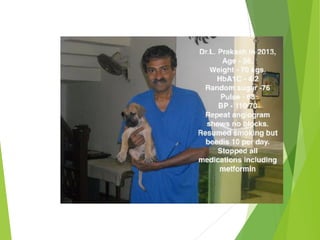
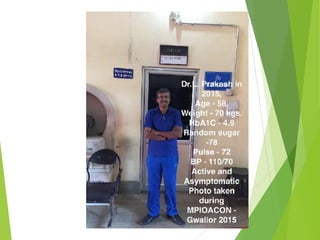
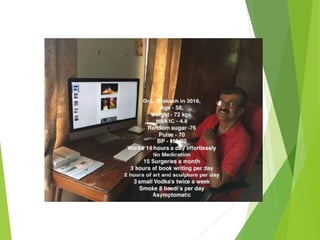
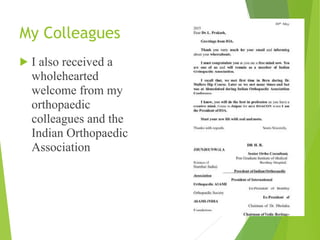
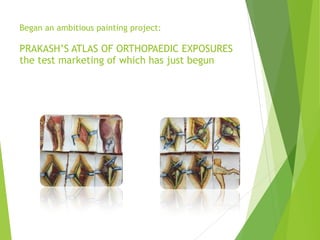
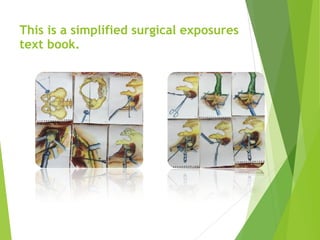
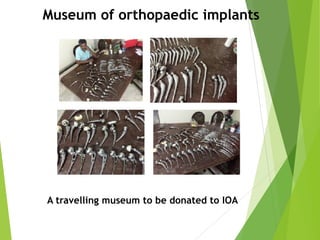
The document details Dr. L. Prakash's thirty years of experience as an orthopaedic surgeon, which can be divided into three phases: as a surgeon (1985-2001), a prisoner (2002-2015), and a teacher/practitioner (2015-present). His imprisonment led him to develop unique orthopaedic practices under severely limited conditions, resulting in innovative treatment methods for various injuries and conditions. The document also includes findings from his studies on conservative treatment efficacy for fractures and spinal issues among inmates, contributing significant insights into orthopaedics in challenging environments.