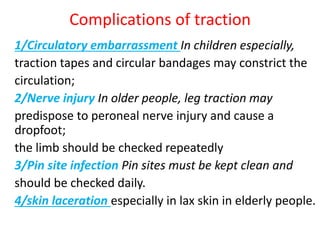
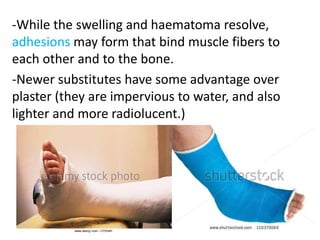
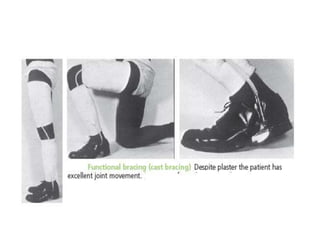
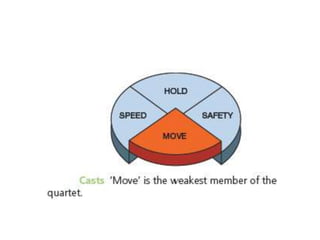
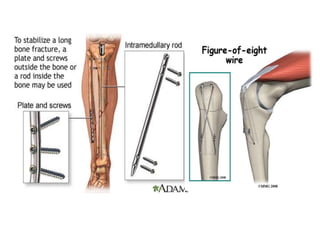
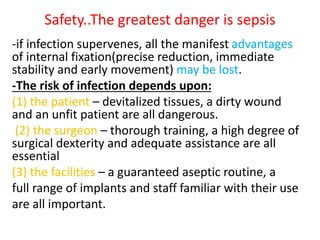
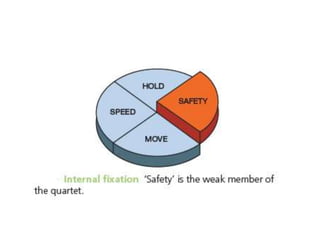
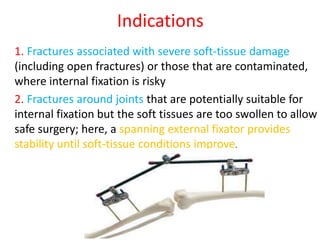
The document outlines the comprehensive treatment of fractures, emphasizing the importance of patient management alongside fracture care. It details various treatment approaches including early measures, reduction techniques, and different methods of holding reductions like casting and internal/external fixation, while also addressing potential complications. Key principles for managing open fractures are also discussed, such as the need for antibiotic prophylaxis, debridement, stabilization, and definitive wound cover.