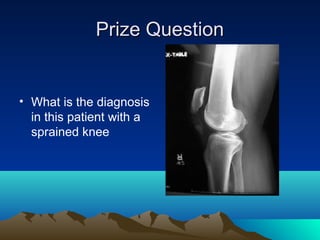
1. Soft tissue MSK injuries like sprains are often diagnosed as "sprains" without determining the specific injury, but a complete physical exam is important.
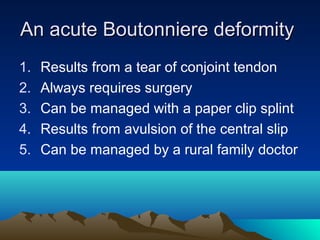
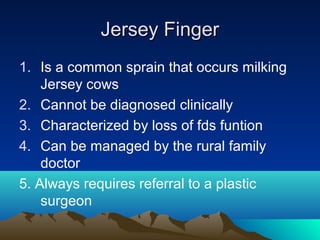
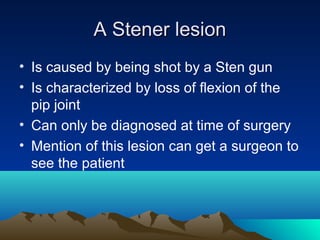
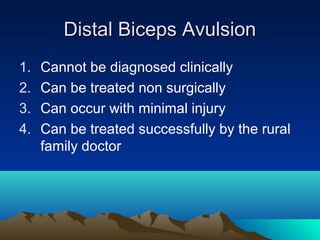
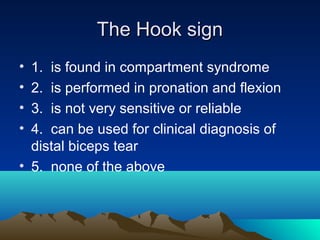
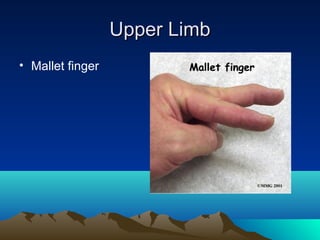
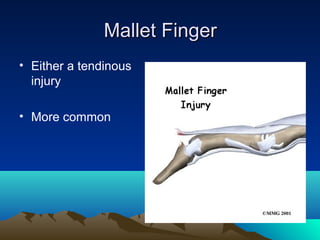
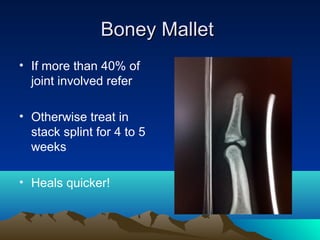
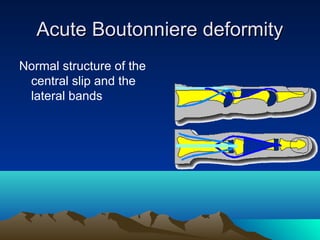
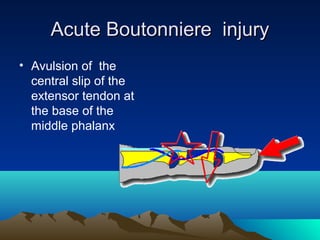
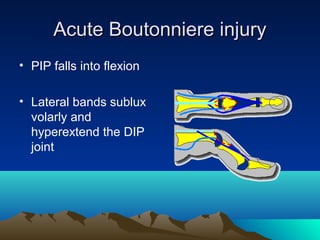
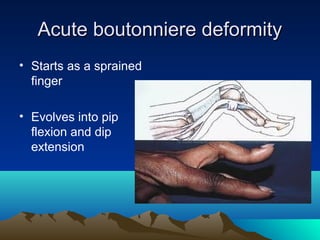
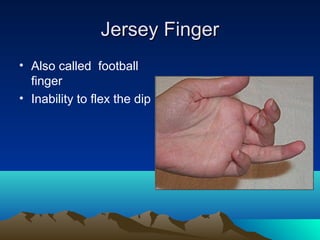
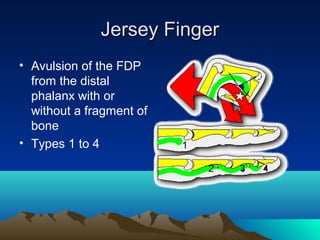
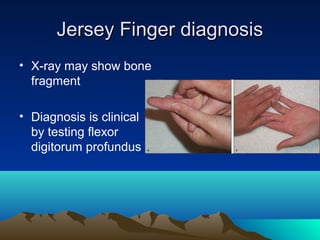
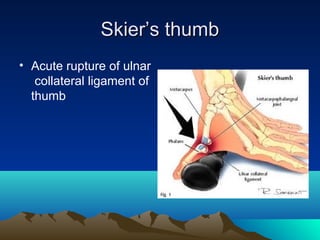
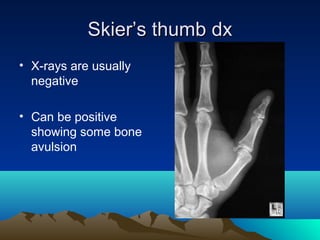
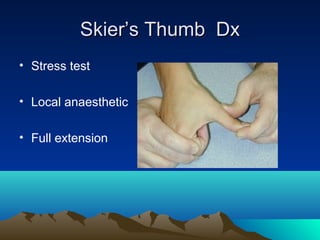
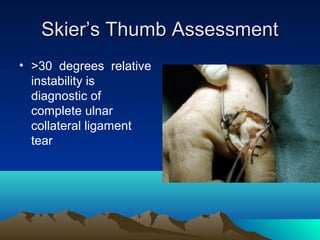
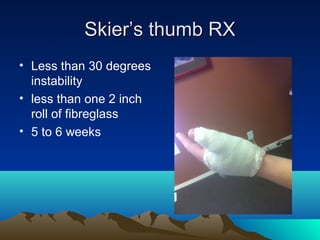
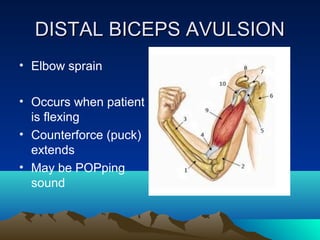
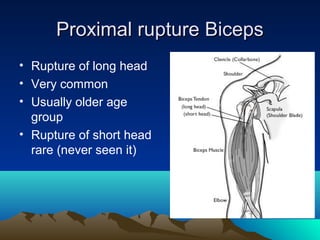
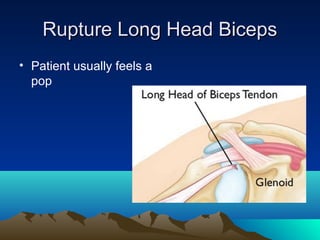
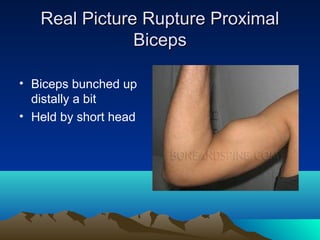
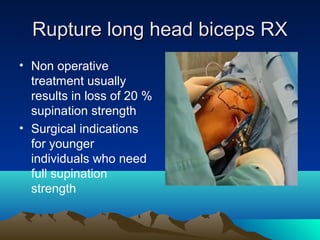
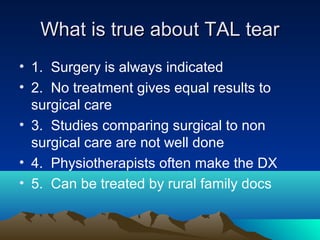
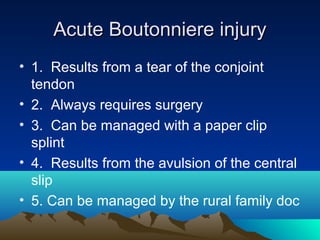
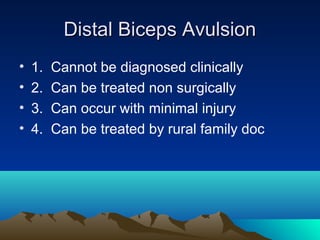
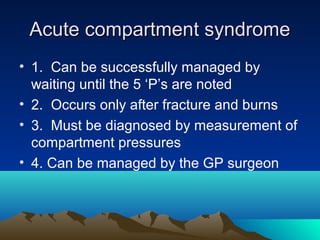
2. Common injuries discussed include mallet finger, boutonniere deformity, jersey finger, skier's thumb, distal biceps avulsion, and ruptured biceps tendon.
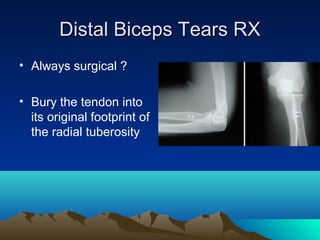
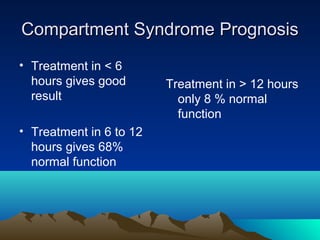
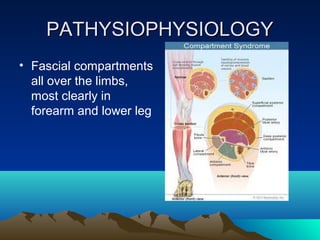
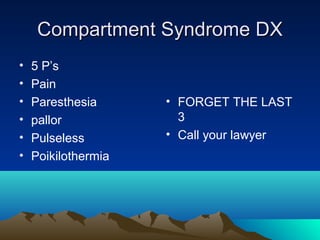
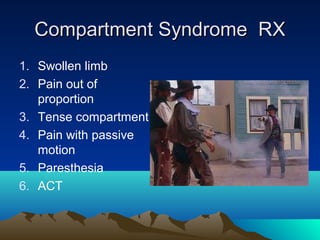
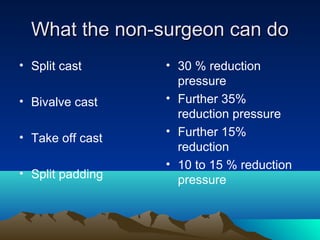
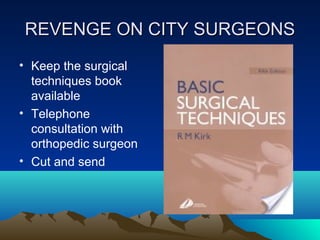
3. Management depends on the specific injury but often involves splinting, casting, or referral for further treatment or surgery depending on the severity. Compartment syndrome is a surgical emergency if not treated promptly.