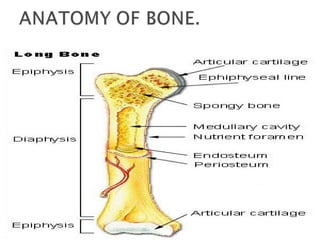
1) Bones provide structure and protection for the body while allowing movement at joints.
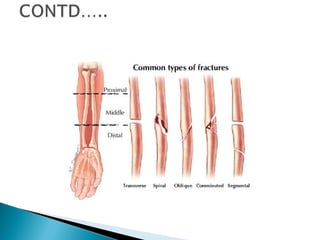
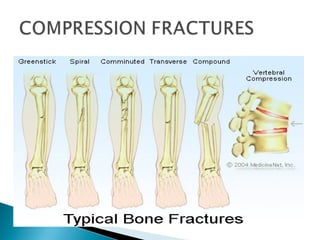
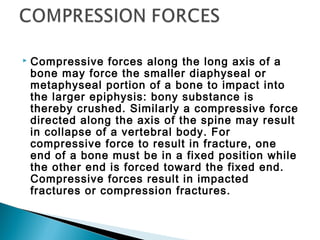
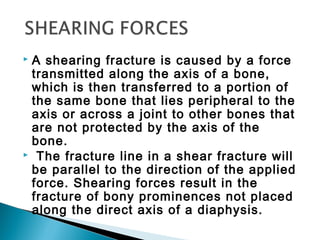
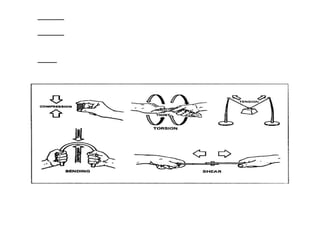
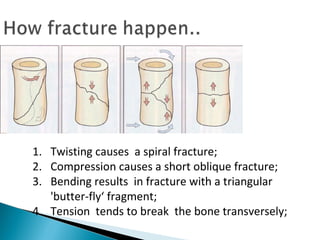
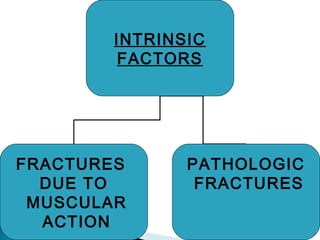
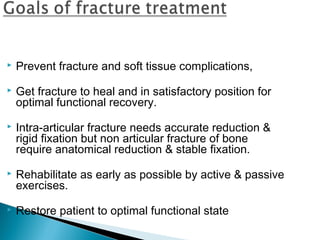
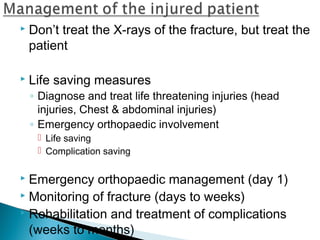
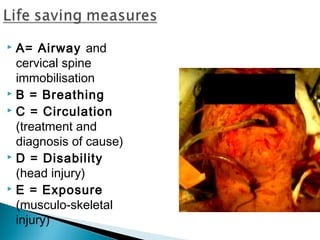
2) Fractures can be caused by direct or indirect forces and result in complete or incomplete breaks in the bone.
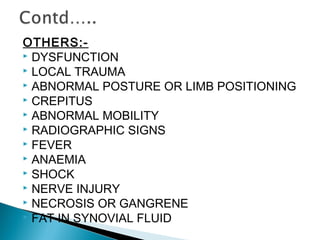
3) Clinical features of a fracture include pain, deformity, loss of function, and crepitus while diagnostic measures include x-rays.