This document provides information on various gynecological surgical procedures including:
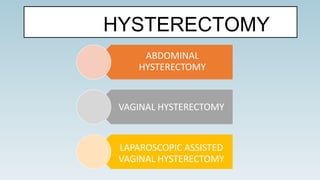
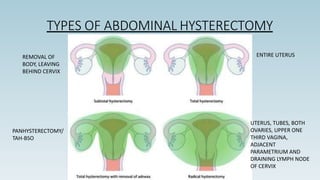
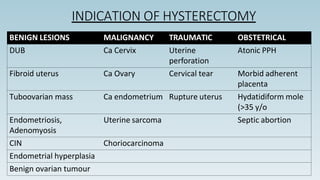
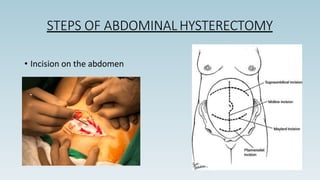
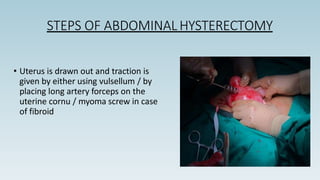
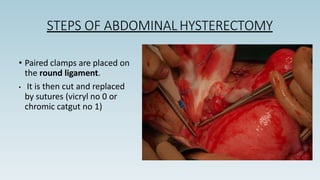
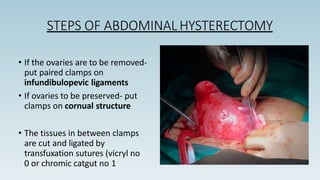
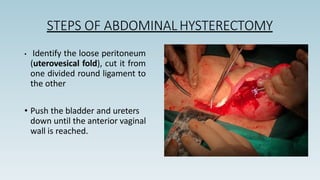
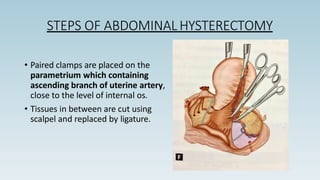
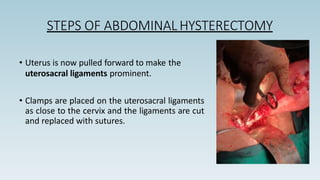
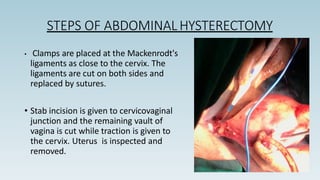
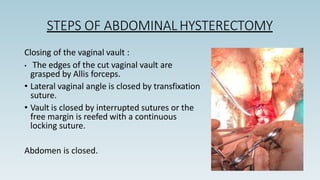
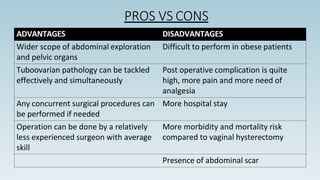
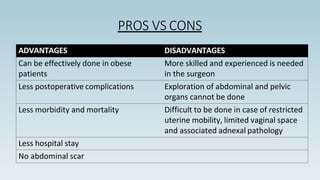
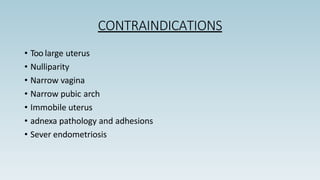
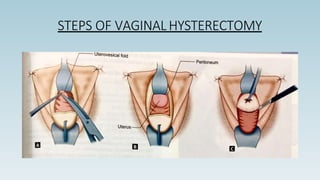
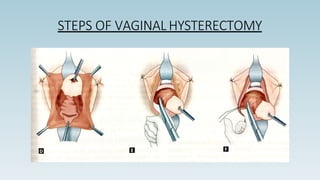
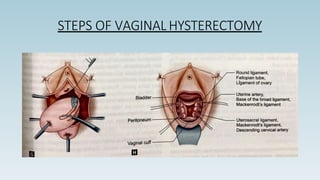
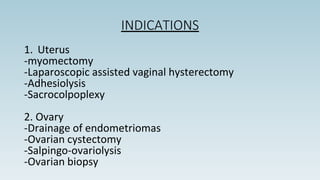
- Hysterectomy - removal of the uterus, described are abdominal and vaginal hysterectomy approaches.
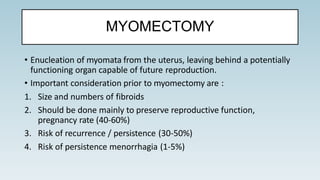
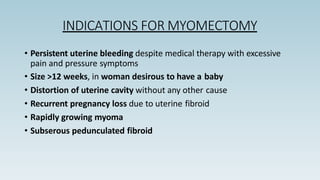
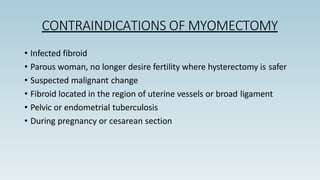
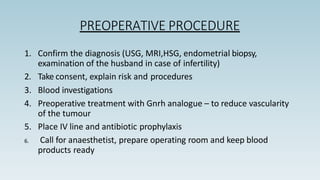
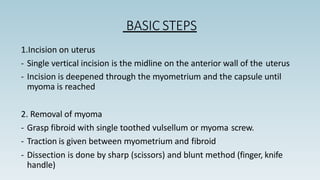
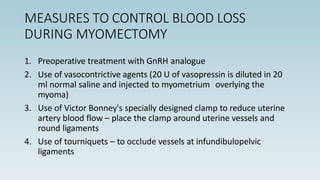
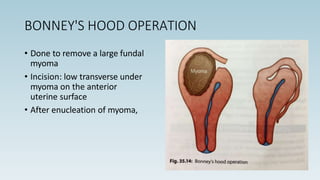
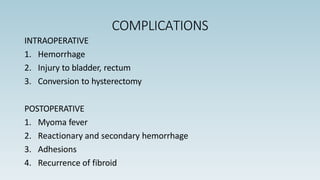
- Myomectomy - removal of uterine fibroids, leaving the uterus intact to preserve fertility.
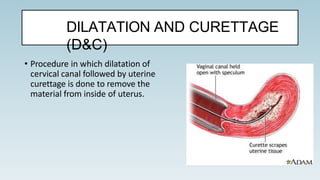
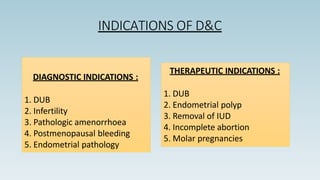
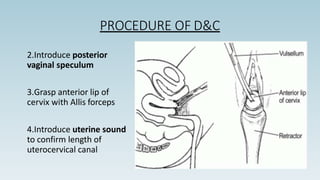
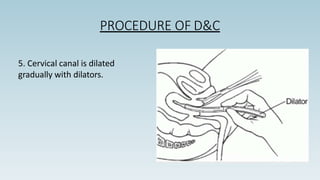
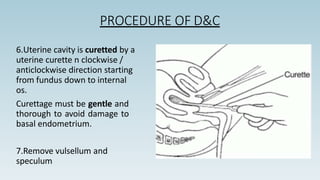
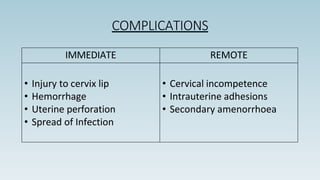
- Dilation and curettage (D&C) - dilating the cervix and scraping the uterine lining, used diagnostically and therapeutically.
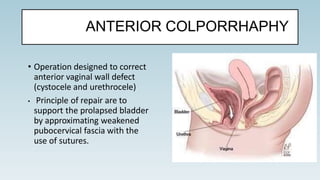
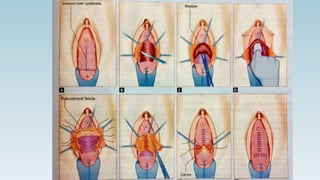
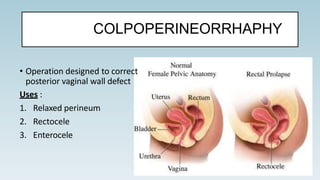
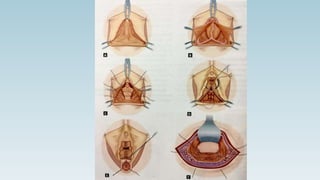
- Anterior and posterior colporrhaphy - procedures to repair vaginal wall defects and prolapse.
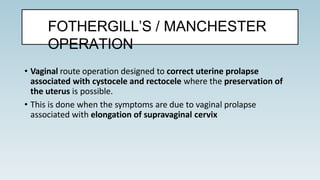
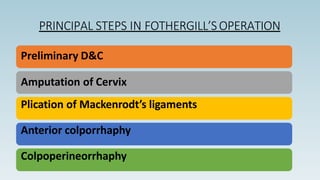
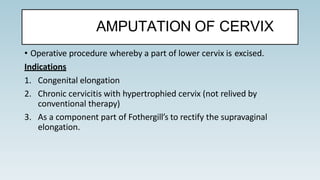
- Fothergill's operation - vaginal procedure to correct uterine prolapse while preserving the uterus.
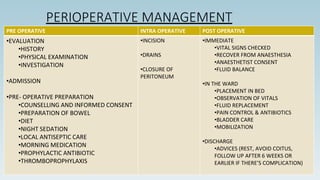
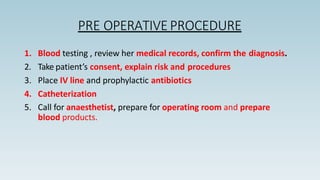
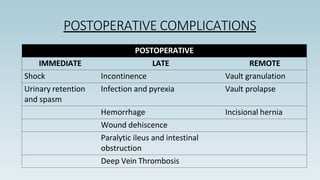
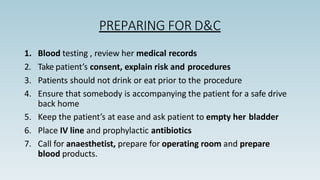
Pre-operative, intra-operative and