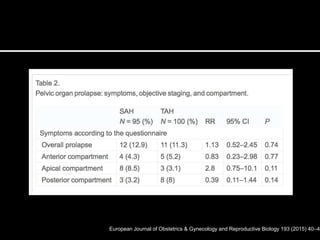
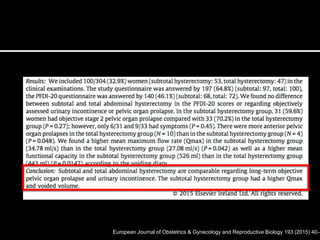
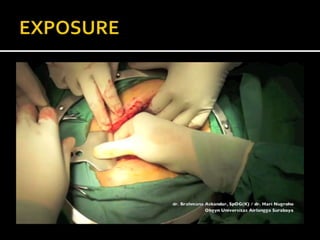
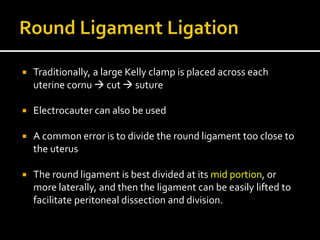
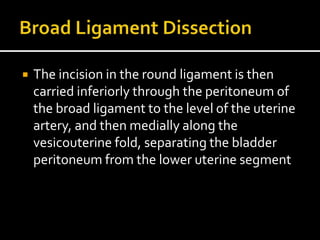
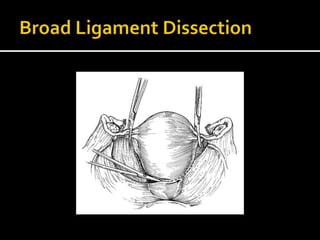
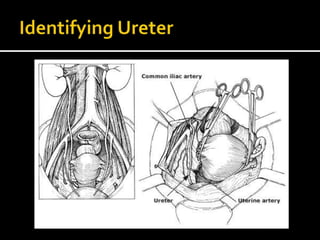
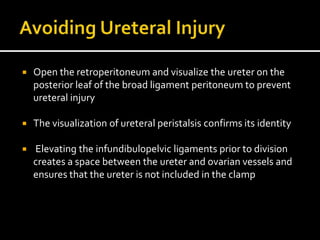
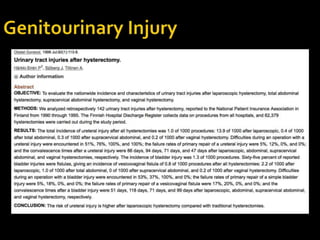
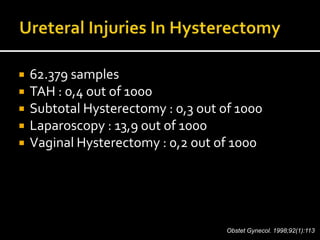
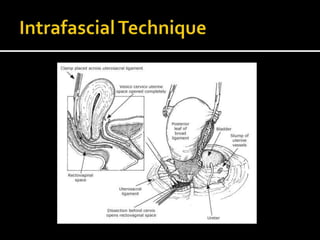
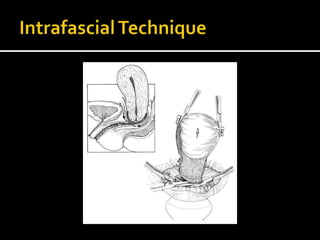
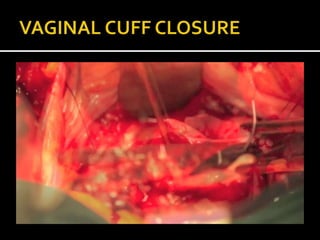
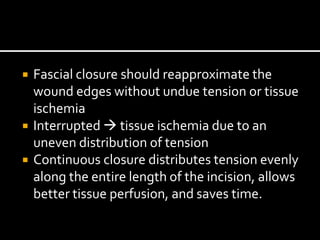
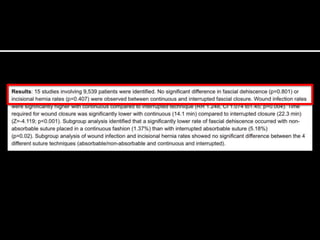
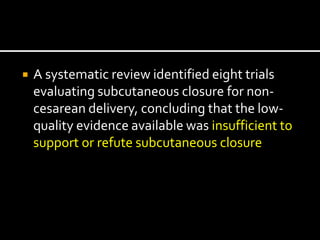
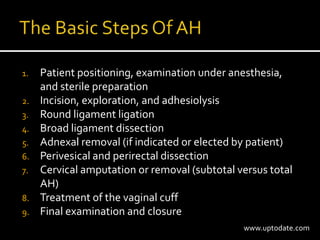
The document discusses various techniques and considerations for performing abdominal hysterectomy, including historical context, types of incisions, and surgical steps involved in the procedure. It highlights the importance of patient counseling, the implications of preserving or removing the cervix, and emphasizes communication between the surgical team, particularly regarding anesthesia. Additionally, it reviews evidence-based recommendations for minimizing complications, including infection prevention and ureteral injury avoidance.