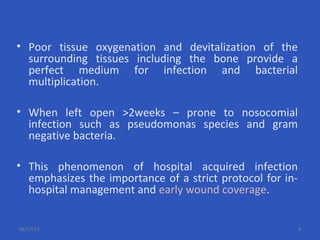
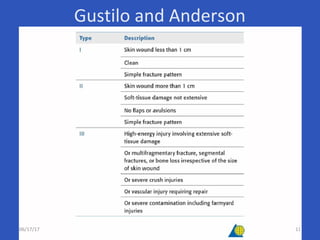
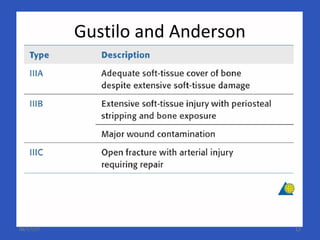
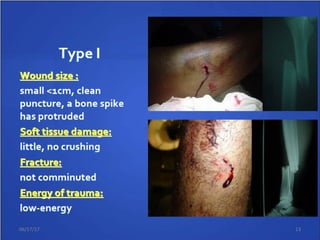
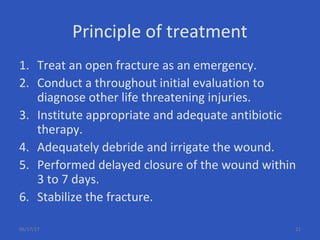
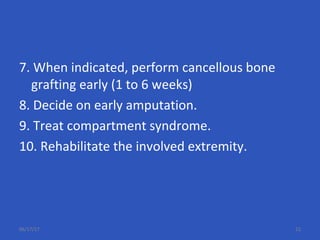
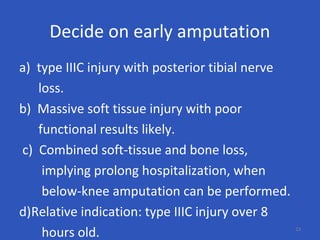
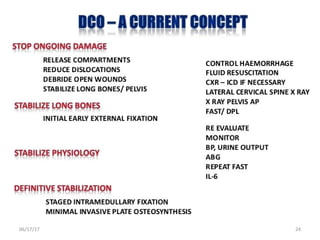
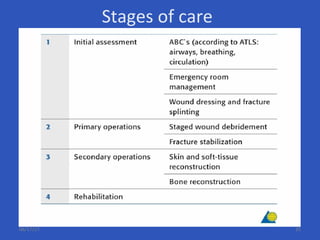
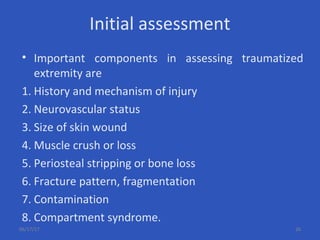
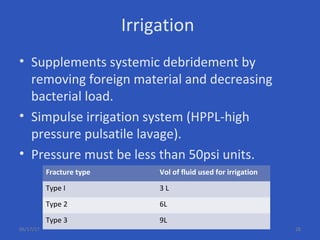
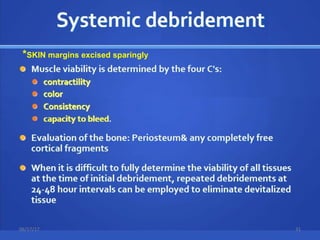
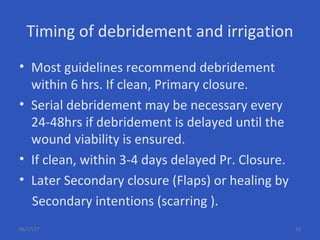
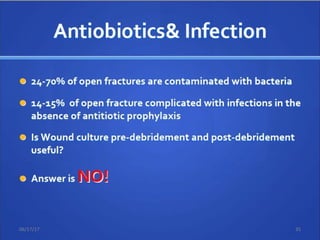
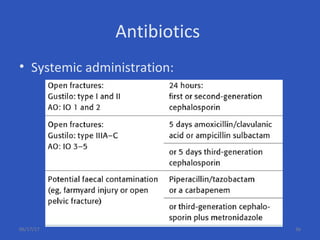
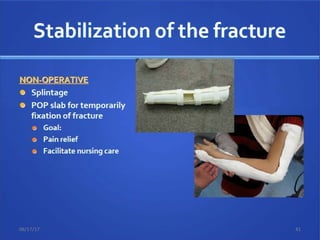
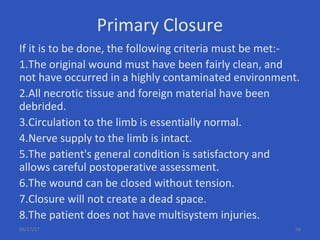
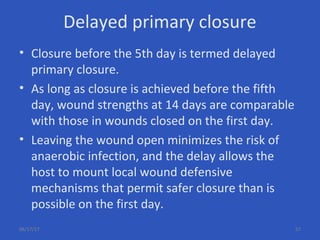
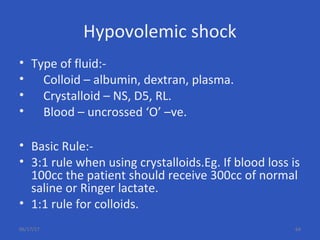
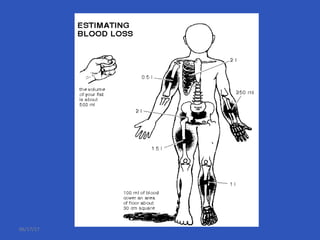
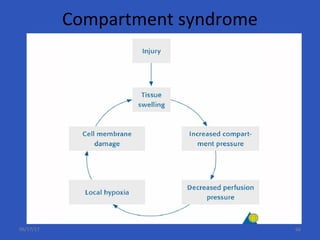
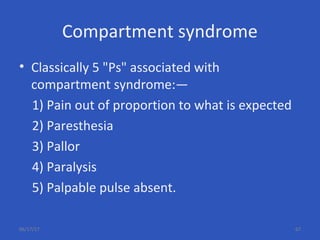
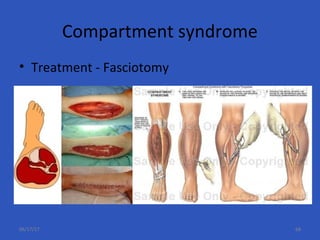
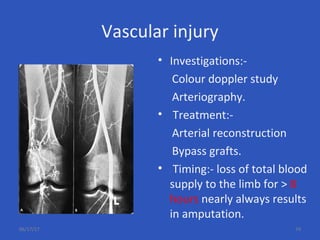
The document provides information on the management of open fractures. It defines open fractures as fractures where there is a breach in the soft tissue envelope exposing the fracture site. Key aspects of management include thorough initial assessment, adequate irrigation and debridement within 6 hours, appropriate antibiotic therapy, and stabilization of the fracture either through external or internal fixation. Complications of open fractures discussed include infection, hypovolemic shock, compartment syndrome, fat embolism, acute respiratory distress syndrome, and neurovascular injuries.