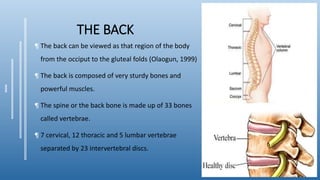
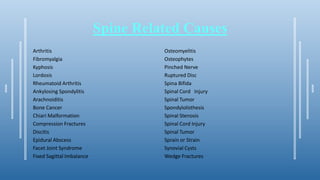
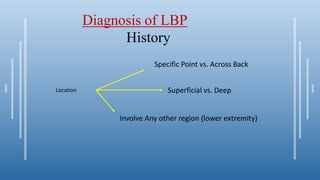
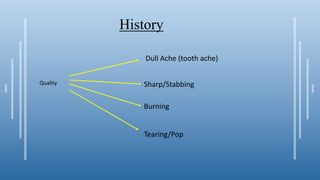
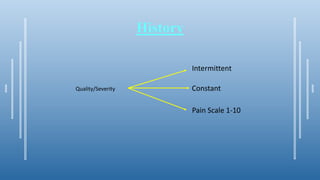
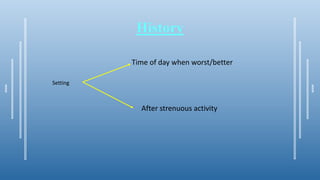
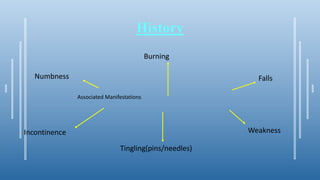
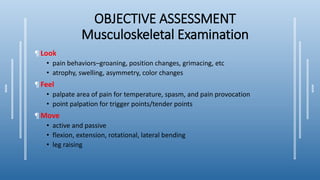
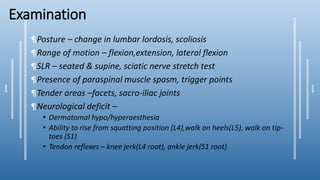
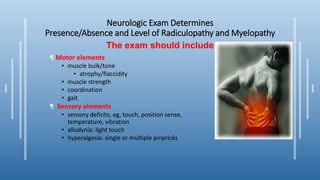
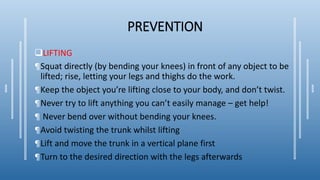
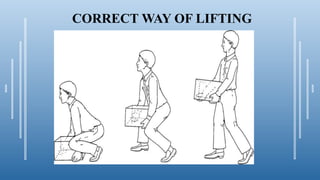
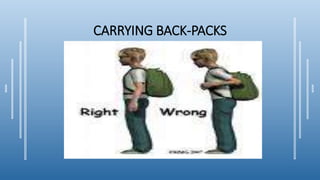
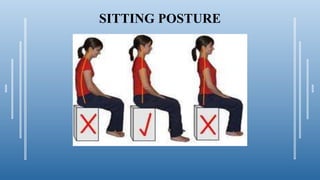
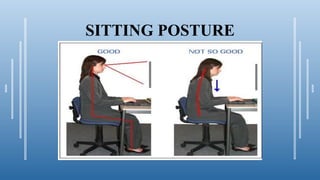
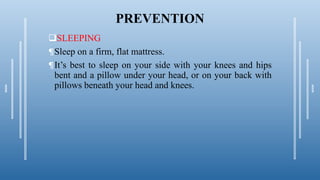
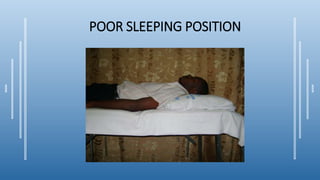
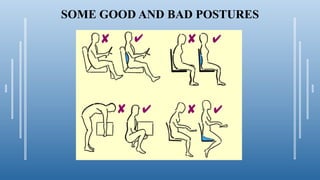
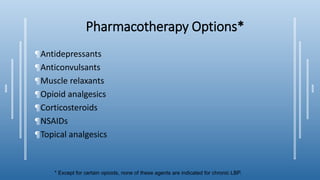
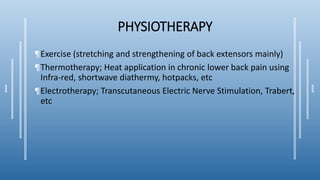
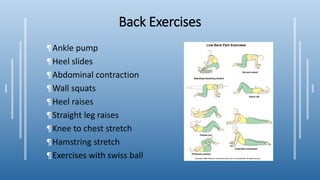
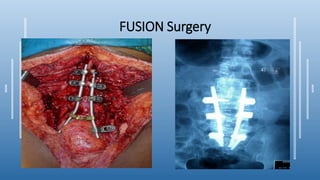
Low back pain is a common condition affecting the lumbar region of the back. It has many potential causes, including muscle strains, injuries to bones or discs, and underlying medical conditions. Diagnosis involves taking a history and conducting a physical exam. Common tests used to evaluate low back pain include x-rays, MRI, and CT scans. Treatment focuses on pain relief through medications, physical therapy, exercise, and in severe cases, surgery. Proper posture and lifting techniques can help prevent low back pain.