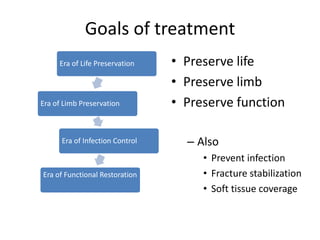
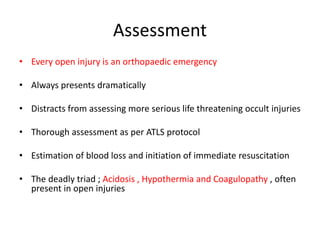
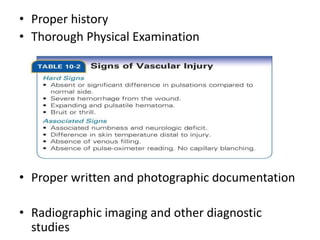
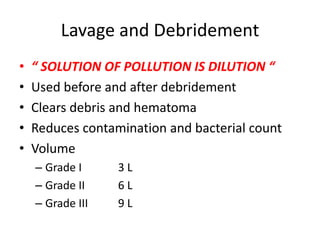
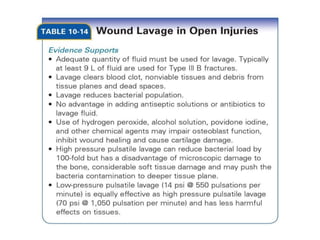
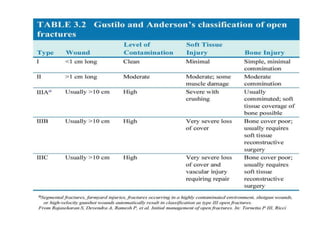
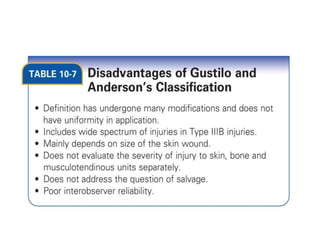
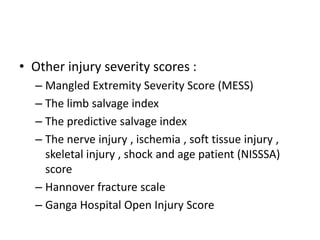
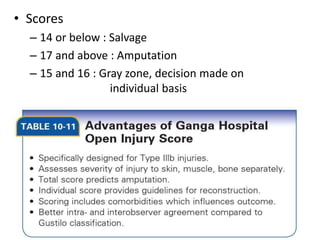
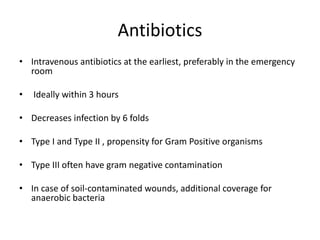
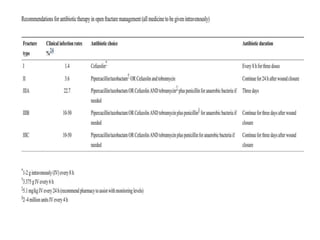
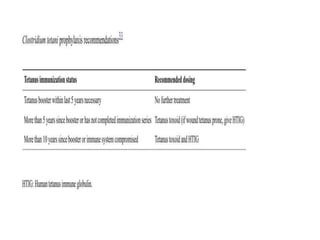
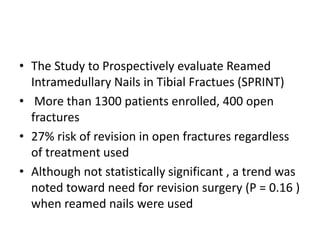
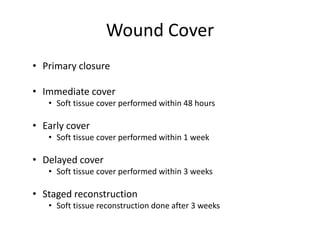
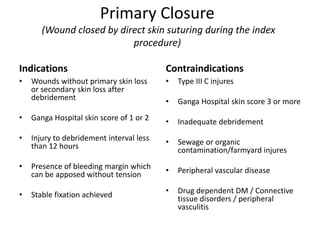
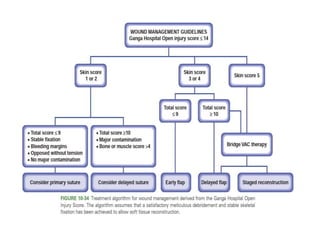
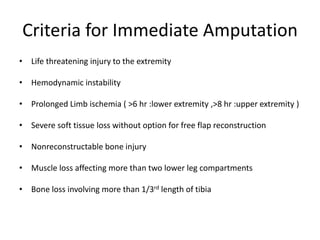
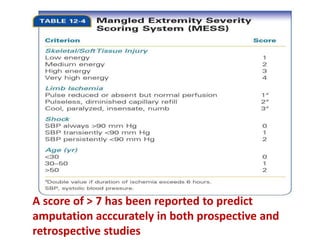
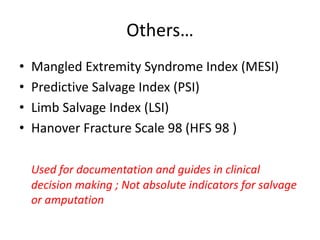
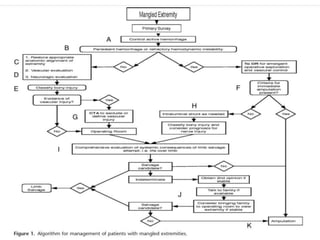
This document discusses open fractures and mangled extremities. It covers the goals of treatment which are to preserve life, limb and function while preventing infection and restoring stability and soft tissue coverage. Open fractures require urgent assessment and debridement to remove non-viable tissue which can be aided by lavage and the use of tourniquets. Skeletal stabilization is also important. Scores can help determine if limb salvage is possible or if amputation is required based on the extent of soft tissue and bone damage. Proper antibiotic use, wound coverage and further reconstruction are also outlined.