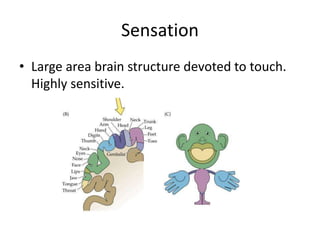
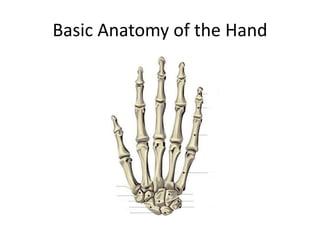
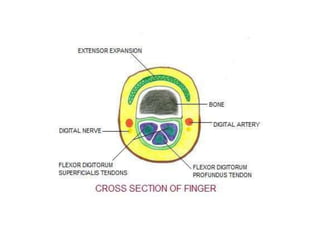
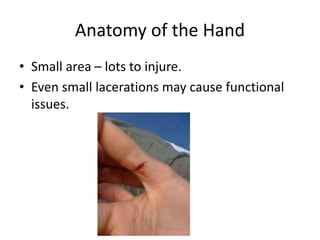
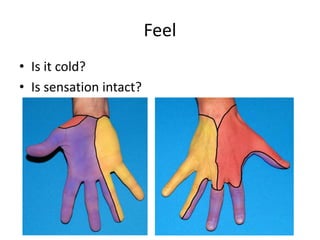
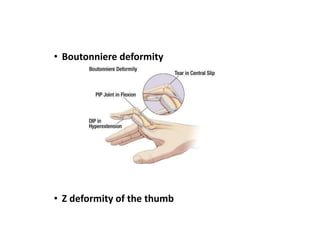
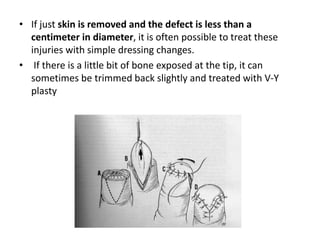
The hand is important for communication, sensation, employment, and independent living. It has complex anatomy with small areas and many structures that can be injured. Common hand injuries include fractures, lacerations, amputations, infections, and bites. Assessing injured hands involves examining for deformities, feeling for sensation and temperature changes, and looking for signs of specific injuries. Many injuries require splinting or surgery followed by hand therapy for recovery. Injuries can have long term functional consequences if not properly treated.