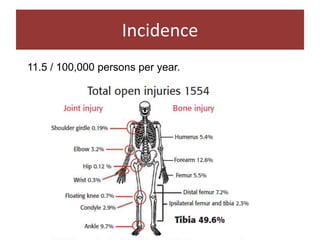
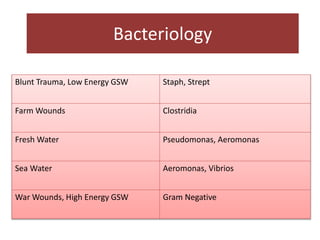
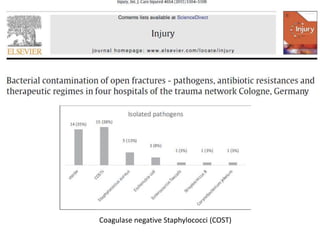
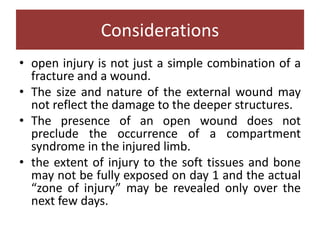
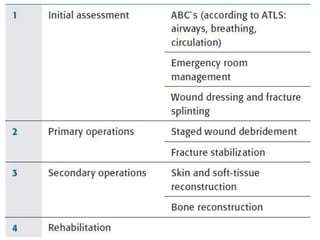
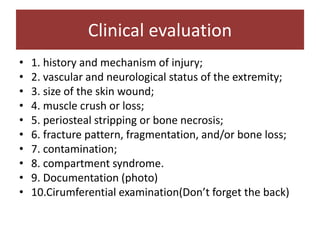
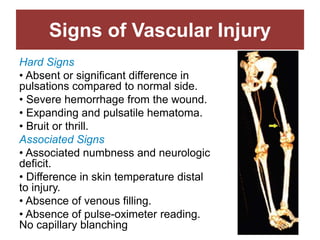
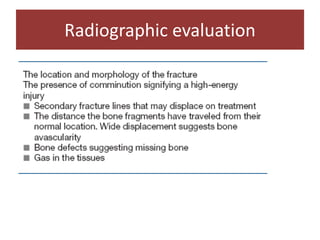
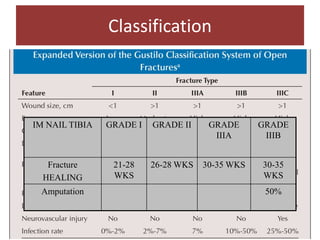
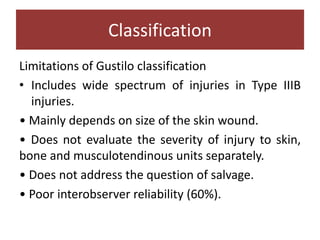
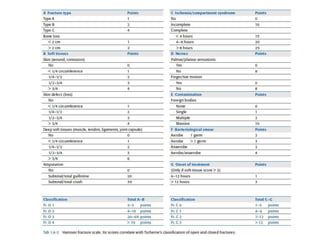
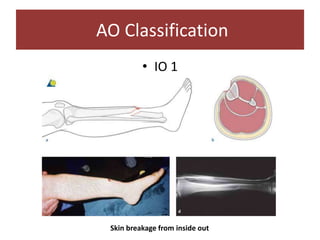
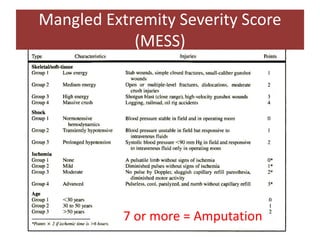
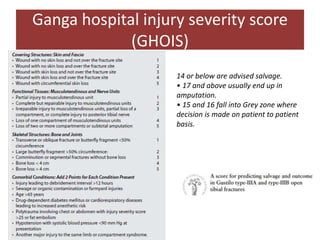
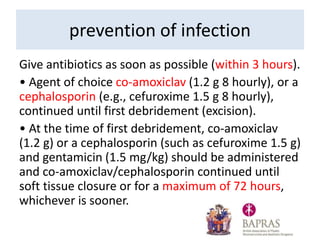
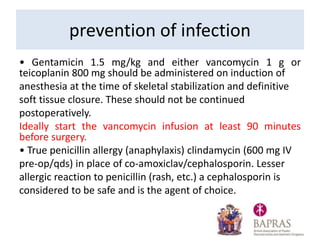
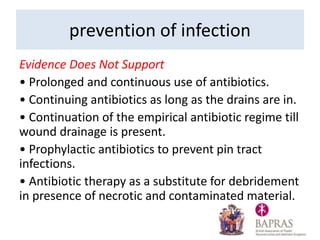
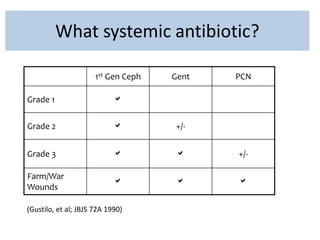
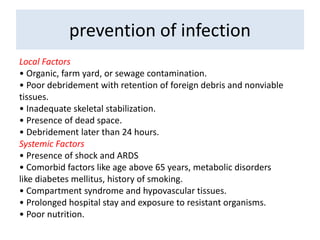
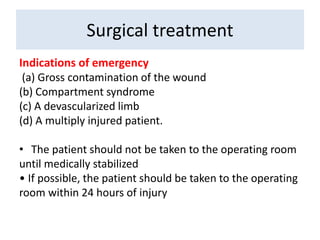
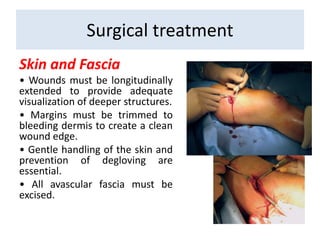
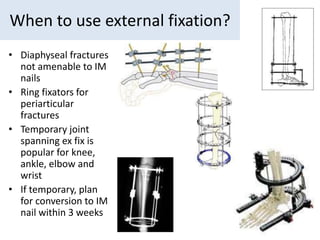
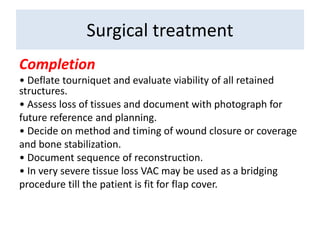
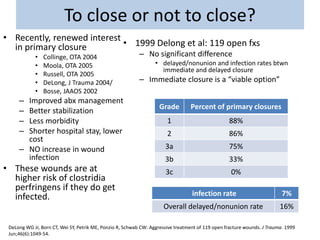
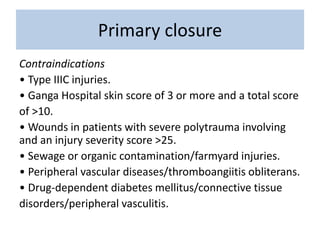
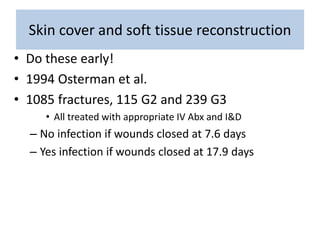
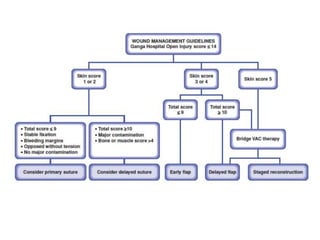
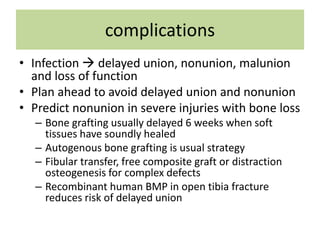
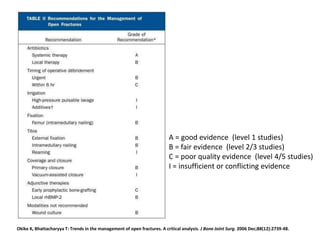
Open fractures are complex injuries that expose bone to contamination and require immediate treatment to prevent infection and promote healing. The management involves assessment of fracture type, soft tissue damage, and contamination level, followed by urgent surgical intervention, including debridement and stabilization. Prompt antibiotic administration and careful monitoring of wound healing are critical to minimize complications such as infection, nonunion, and amputation.