Intellectual disability is complex and affects each person differently. It involves below average cognitive ability and difficulties in areas of functioning that are present from childhood. While IQ provides a measure of cognitive ability, it does not define the whole person or their needs. Providing support requires understanding each individual's unique profile of abilities, circumstances, and how intellectual disability impacts them.









![Communication disorders
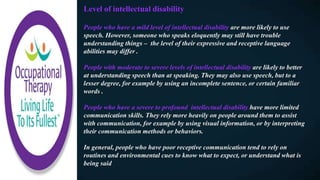
There is a higher rate of sensory, physical and neurological disabilities amongst
people with an intellectual disability . These can all have an impact on
communication.
For example, communication difficulties are commonly associated with autism
spectrum disorders. Some features of this could be:
- Not speaking
- Difficulty with social aspects of communication
- Use of idiosyncratic (personally developed) language.
In other cases, the physical aspects of a developmental disability may have an
impact on expressive communication. For example, people with cerebral palsy
may not have enough neuromuscular control to speak or articulate words [2].
Having an intellectual disability is associated with higher risk of hearing
impairment and vision impairment , adding an additional barrier to
communication. It’s important to remember that, having difficulties with
communication does not mean that someone does not have the capacity to
understand and make decisions](https://image.slidesharecdn.com/010-180627235457/85/Occupational-Therapy-and-Intellectual-Disability-32-320.jpg)