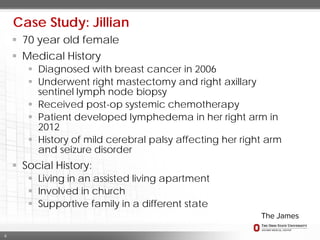
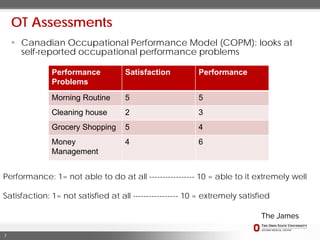
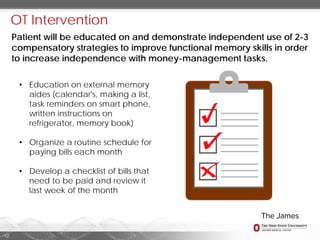
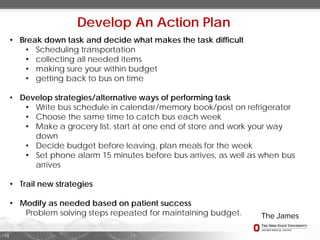
Occupational therapy aims to help cancer patients achieve maximum functional independence despite their prognosis. For a 70-year-old woman with breast cancer, chemotherapy caused fatigue, cognitive issues, and lymphedema. Occupational therapy assessed her difficulties with activities of daily living, instrumental activities, and leisure due to fatigue. Interventions included energy conservation strategies, activity modifications, external memory aids, and problem-solving training to improve independence with tasks like morning routines, chores, grocery shopping, and bill paying. The patient demonstrated reduced fatigue and improved cognitive function and satisfaction with occupational performance after therapy.