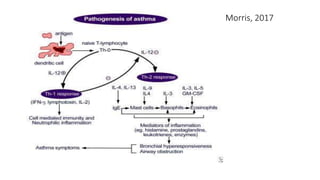
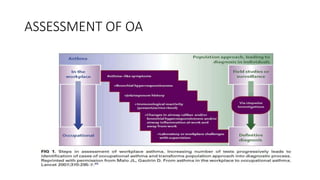
The document discusses occupational lung diseases, including their causes, types, diagnosis, and management. Some key points:
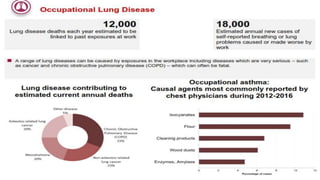
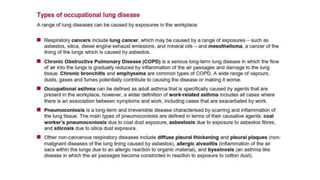
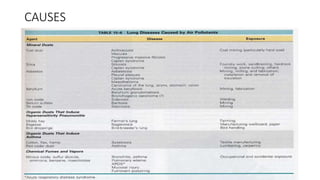
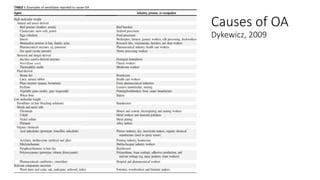
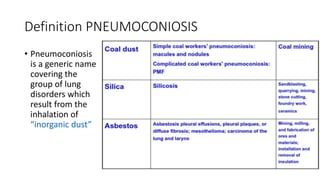
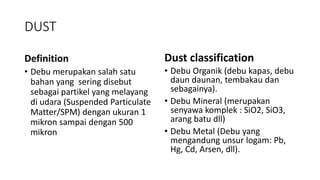
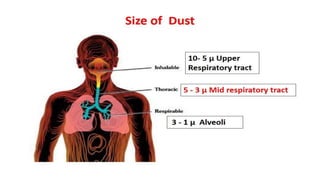
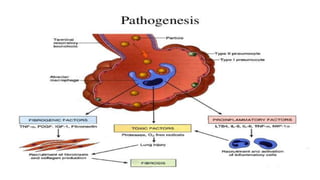
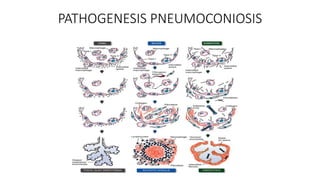
1. Occupational lung diseases are caused by inhaling dusts, chemicals, or proteins at work. Pneumoconiosis refers specifically to diseases from inhaling mineral dust.
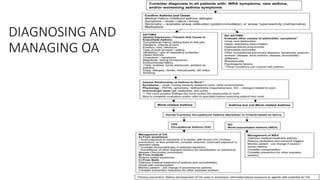
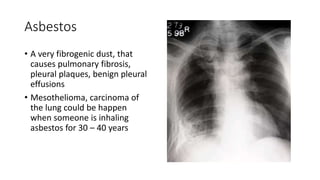
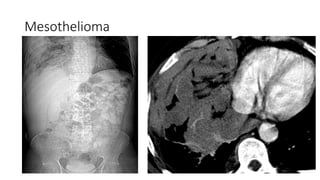
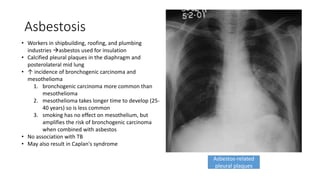
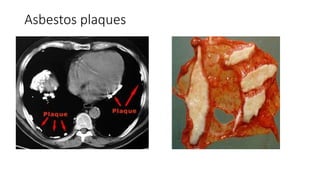
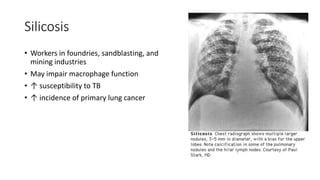
2. Major causes of occupational lung disease include occupational asthma, pneumoconiosis like silicosis and asbestosis, and mesothelioma from asbestos exposure.
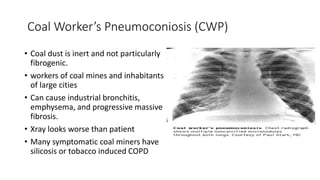
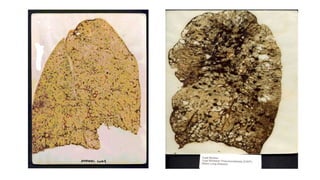
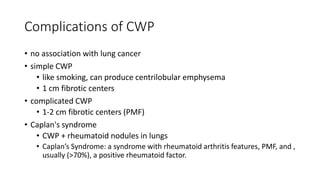
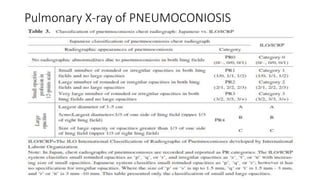
3. Pneumoconiosis is classified as major, minor, or benign depending on the severity of lung fibrosis. Major types include asbestosis, silicosis, and coal worker's pneumoconiosis.
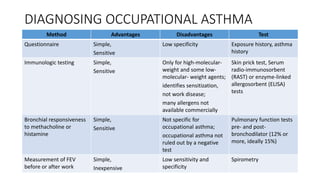
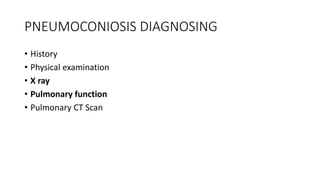
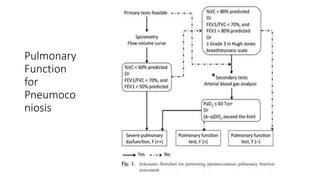
4. Diagn