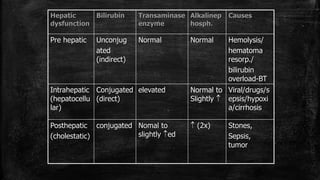
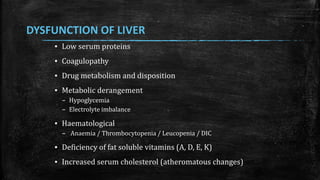
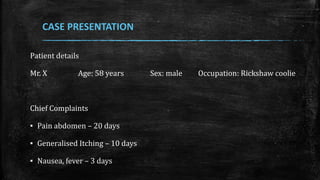
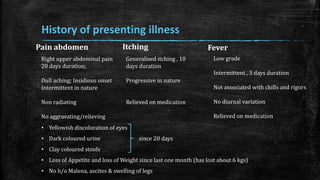
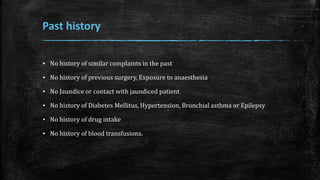
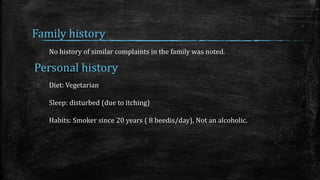
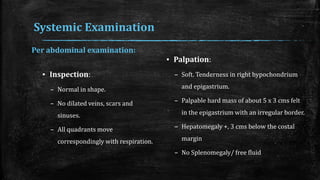
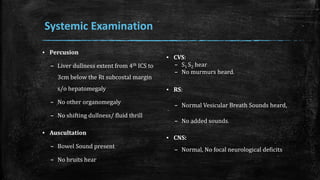
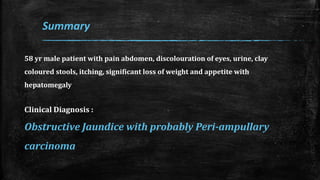
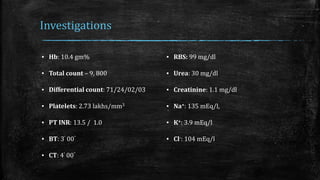
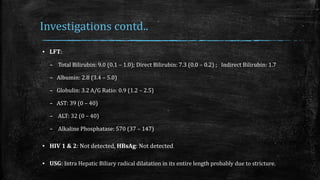
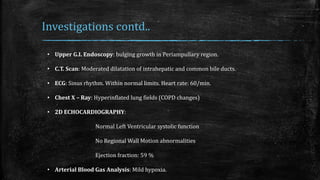
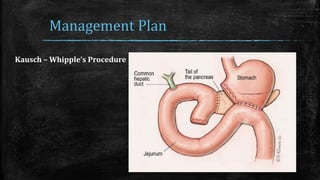
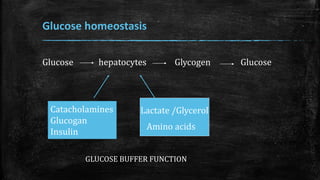
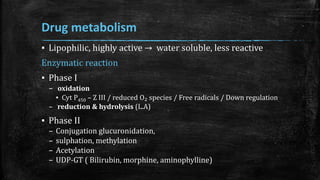
The document presents a clinical case of a 58-year-old male with obstructive jaundice, characterized by abdominal pain, jaundice, clay-colored stools, and significant weight loss. Investigations indicated suspected peri-ampullary carcinoma with intrahepatic biliary dilation, prompting a diagnosis leading to a management plan involving a Kausch-Whipple procedure. The document further discusses liver physiology, pathophysiology of jaundice, and drug metabolism in the context of liver function.
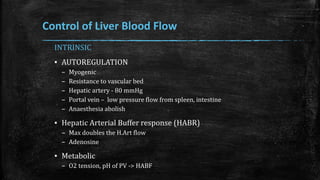
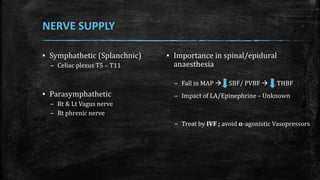
![▪ Portal vein – only α receptor
▪ Hep artery – α/β present
▪ Importance
– Dopamine [DOC]
– Dobutamine
– Noradrenaline](https://image.slidesharecdn.com/obstructivejaundiceanaesthesia-161025113529/85/Anaesthetic-management-in-Obstructive-jaundice-23-320.jpg)
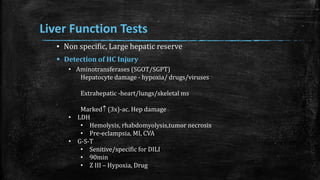
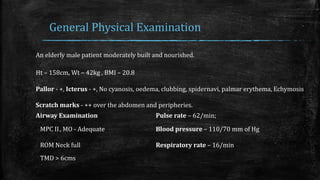
![Clearance of drugs from plasma
Rowland's Equation
▪ Hepatic Clearance: Cl(h) = Q [(f x Clint)/(Q+ f x Clint)]
▪ Q = hepatic blood flow
▪ f = fraction of free drug (not bound)
▪ Clint = intrinsic capacity of the hepatocytes to metabolize a drug
▪ High DER ∝ Rapid clearance
– Consider ER is 1, Now Cl = Q [ DER – Drug Extraction Ratio ]
▪ Low DER ∝ Low clearance
– Capacity limited / extract less avidly
– By protein binding , Hepatic enzymes](https://image.slidesharecdn.com/obstructivejaundiceanaesthesia-161025113529/85/Anaesthetic-management-in-Obstructive-jaundice-39-320.jpg)