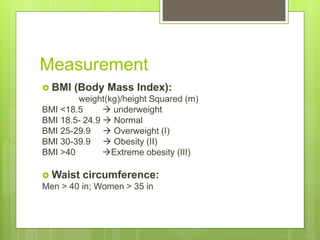
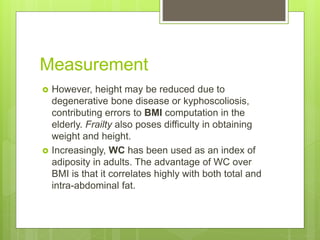
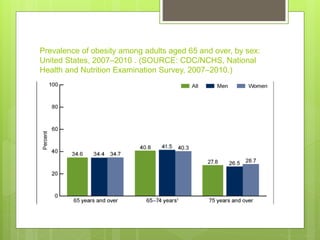
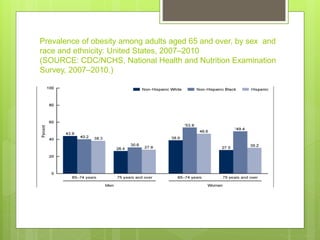
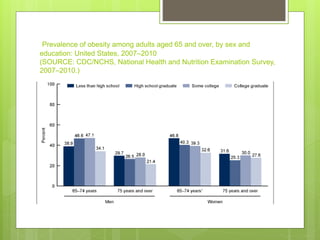
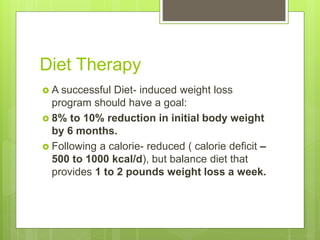
The document discusses obesity in elderly populations, highlighting its definition, measurement, prevalence among various demographics, and the associated health risks and comorbidities. It emphasizes that obesity results from an imbalance in energy intake and output, particularly as physical activity decreases with age, and outlines the implications of weight loss in older adults. Recommendations for lifestyle interventions, diet, exercise, pharmacotherapy, and bariatric surgery are also provided, noting that careful consideration is necessary when addressing obesity in the elderly.