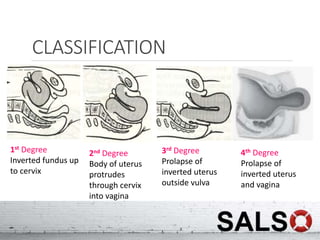
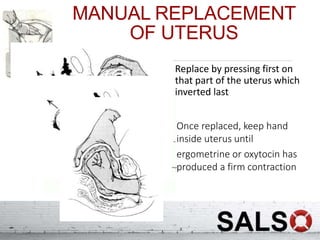
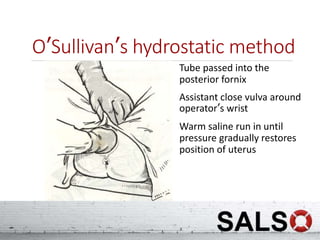
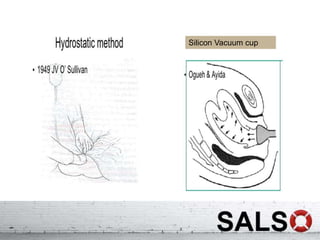
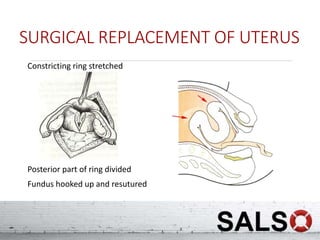
Uterine inversion occurs when the uterus turns inside out, most commonly during delivery from excessive cord traction or fundal pressure. It can range from the fundus inverting into the cervix to the entire uterus prolapsing outside the body. Prompt diagnosis and management is needed to prevent shock. The uterus must be manually or surgically replaced before detaching the placenta to avoid hemorrhage. Prevention involves controlled cord traction and avoiding fundal pressure until the placenta separates naturally.