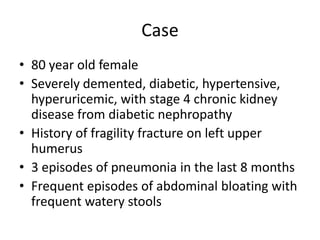
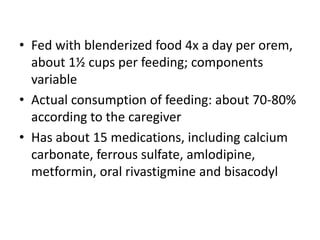
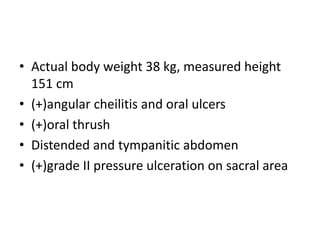
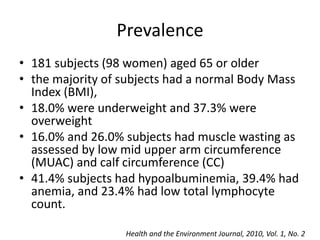
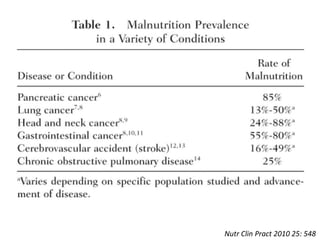
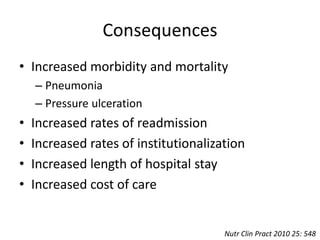
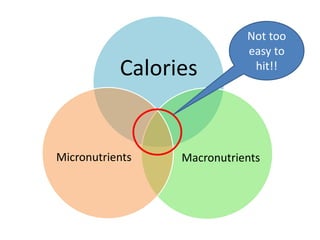
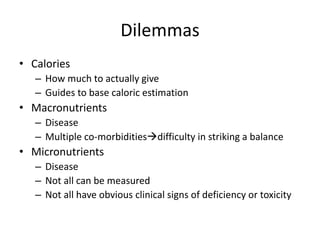
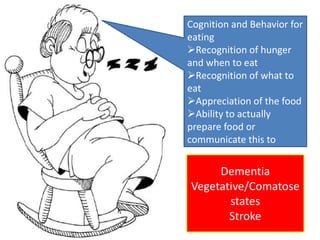
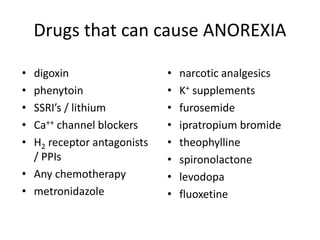
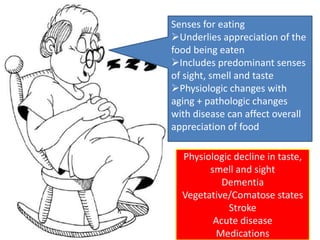
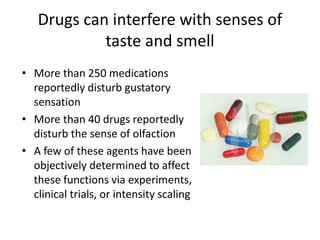
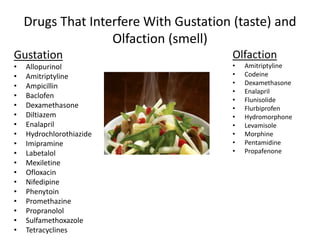
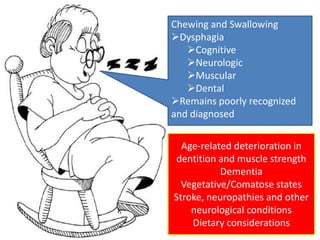
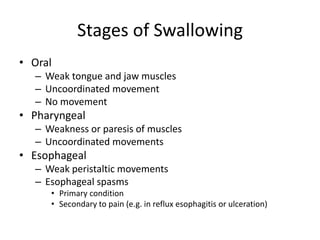
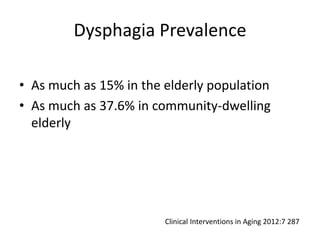
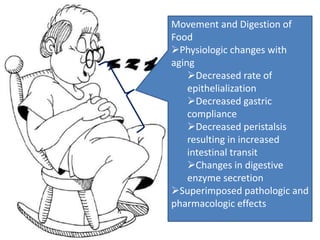
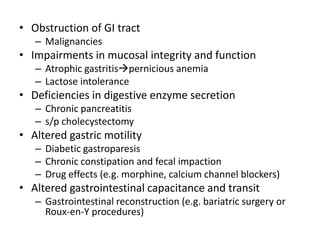
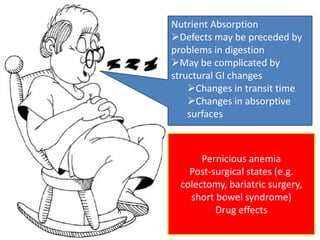
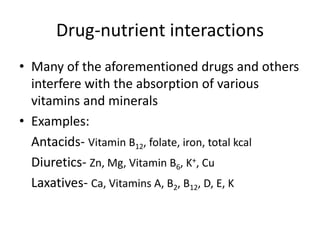
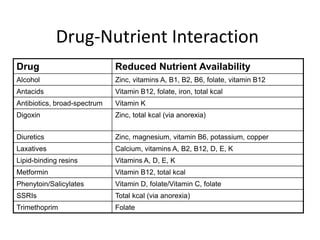
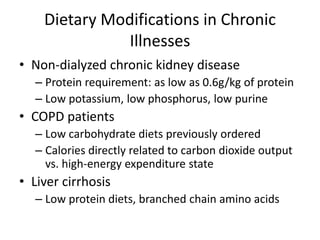
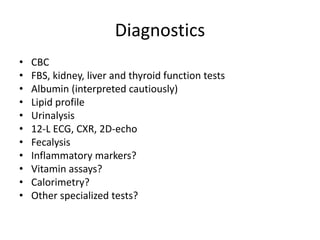
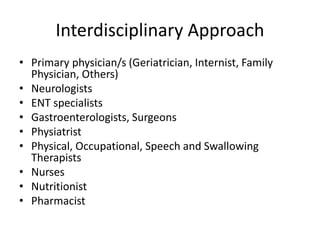
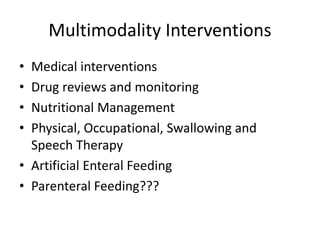
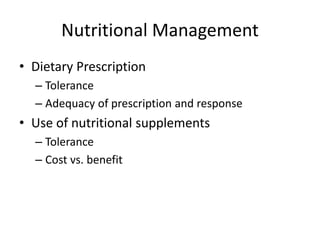
This document discusses nutritional disorders that are common in patients with chronic illness. It notes that malnutrition can result from problems at different stages of the nutrition pathway, including cognition/behavior, senses, chewing/swallowing, digestion, absorption, and nutrient metabolism. Common chronic conditions like dementia, kidney disease, and constipation can all contribute to poor nutrition. An interdisciplinary approach is needed to properly assess, diagnose, and manage nutritional disorders through medical, dietary, and rehabilitation interventions.