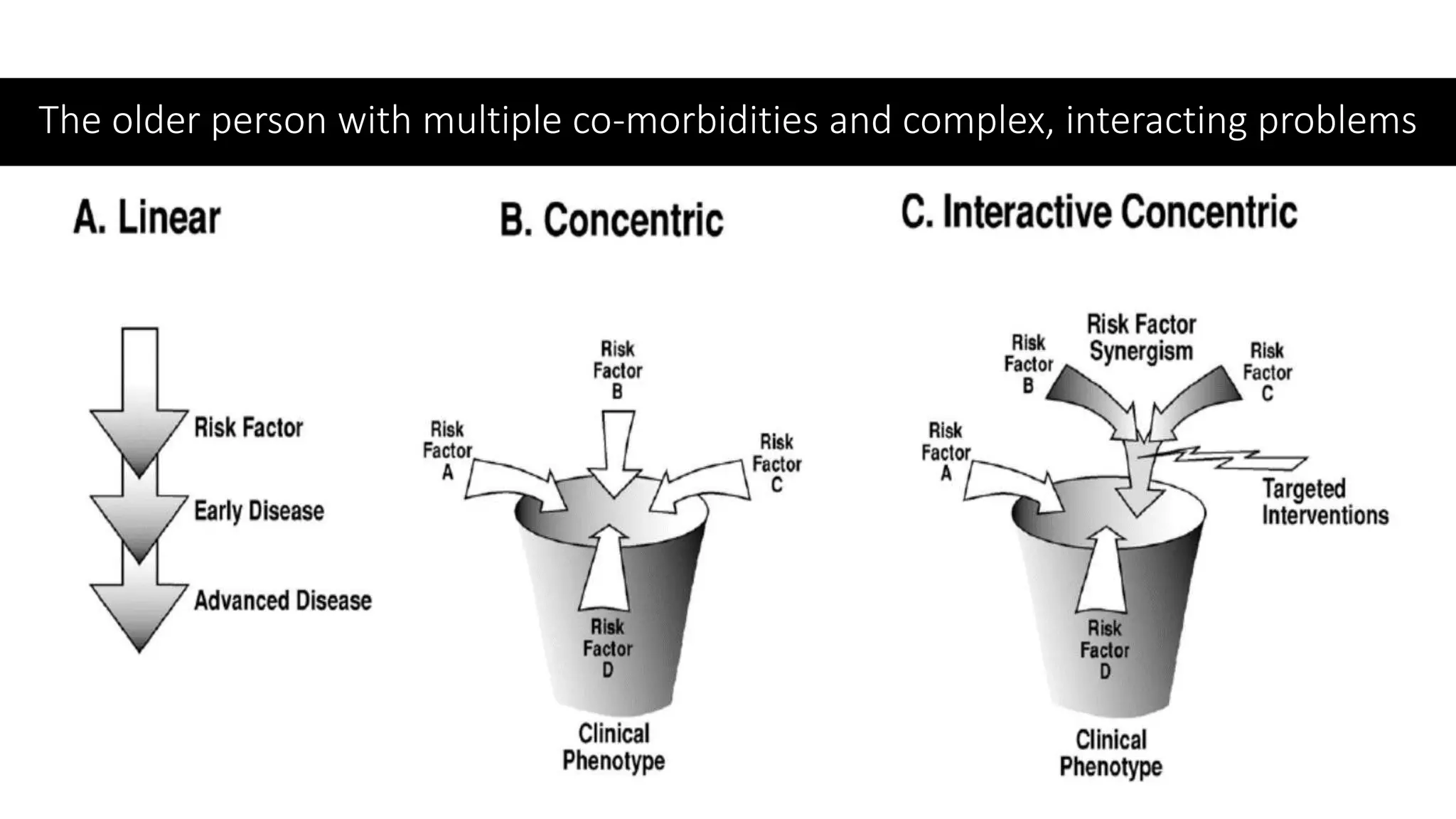
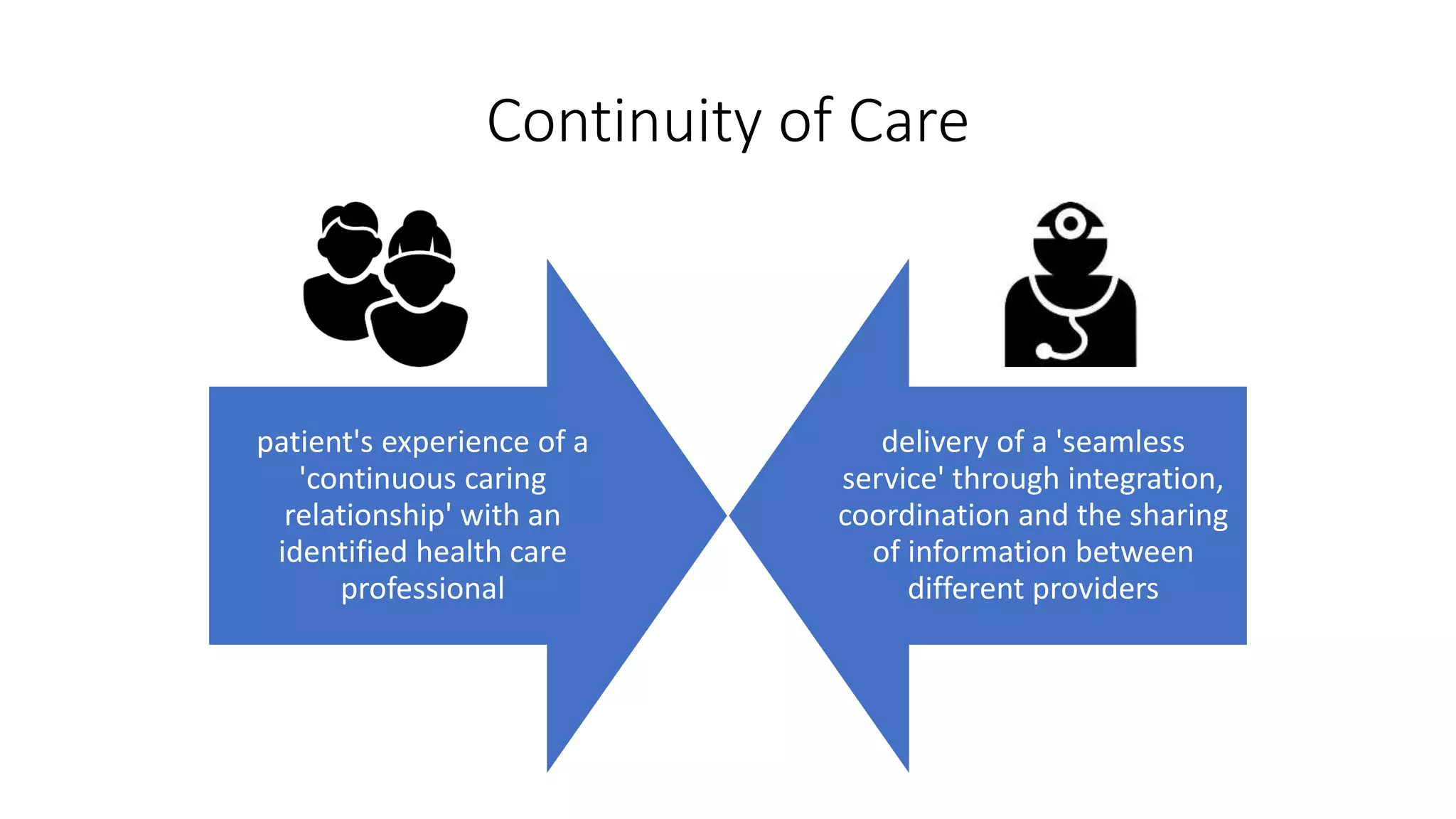
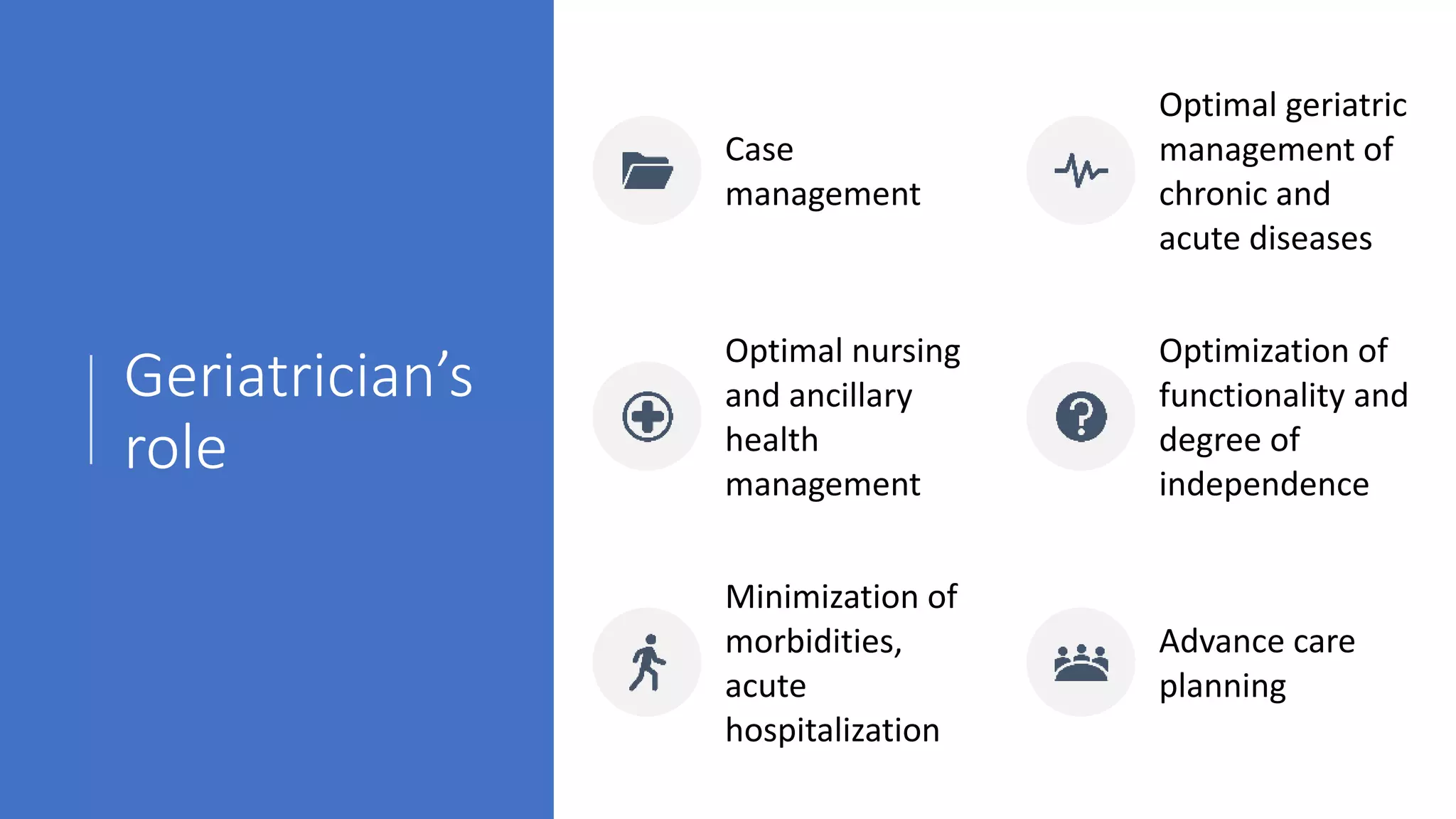
A geriatrician is a primary care doctor with specialized training in treating older patients. They can coordinate overall care, manage all health issues of older patients through comprehensive geriatric assessments, and design care plans to address multiple conditions. Referral to a geriatrician is recommended for older patients with complex medical issues, peculiar manifestations of diseases, frailty, polypharmacy management, discharge planning, continuity of care including home care, palliative care, and institutional care needs. Their role includes managing complex comorbidities, investigating atypical symptoms, rationalizing medications, ensuring smooth care transitions, and optimizing functionality and independence.