This document discusses the comprehensive geriatric assessment (CGA). It begins by defining the CGA as a multidimensional, interdisciplinary diagnostic process that develops a coordinated treatment plan emphasizing quality of life, functional status, and prognosis.
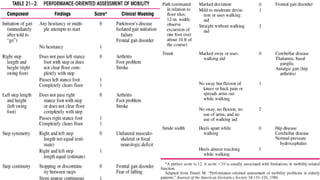
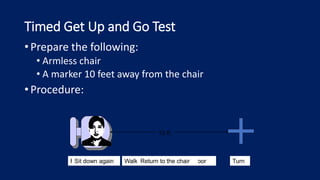
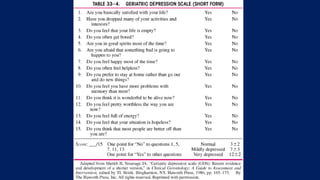
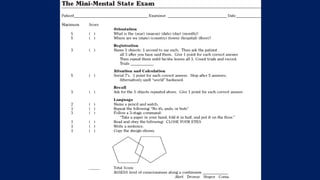
It then identifies the key components of a CGA as including medical history, physical and functional status, behavioral and emotional status, environmental and social support, and spiritual well-being. Common tools used include assessments of activities of daily living, cognition, nutrition, and fall risk.
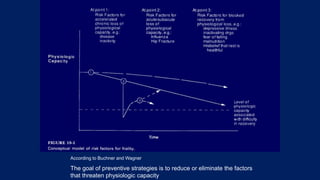
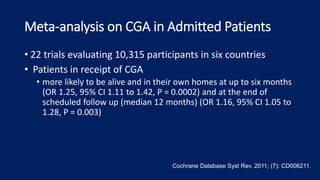
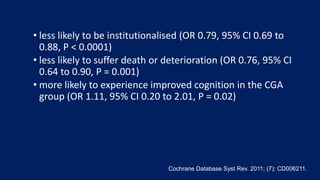
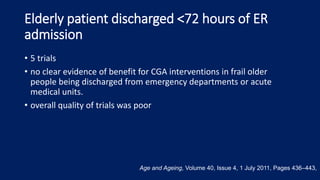
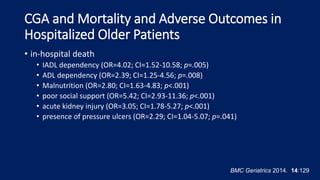
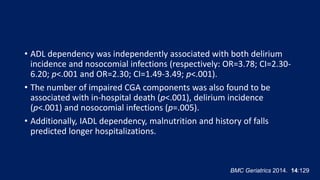
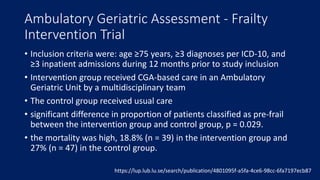
The document explains that a CGA is recommended for older adults who are frail or have geriatric syndromes like falls or polypharmacy. Evidence shows that CGA can reduce mortality, institutionalization














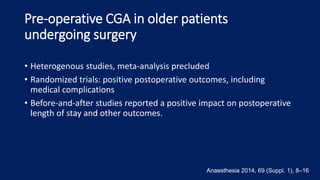
![Proactive care of older people undergoing surgery
('POPS’)
• 2 cohorts of elective orthopaedic patients (pre-POPS vs
POPS, N =54)
• POPS group
• fewer post-operative medical complications including pneumonia
(20% vs 4% [p = 0.008]) and delirium (19% vs 6% [p = 0.036])
• significant pressure sores (19% vs 4% [p = 0.028]), poor pain
control (30% vs 2% [p<0.001]), delayed mobilisation (28% vs 9% [p
= 0.012]) and inappropriate catheter use (20% vs 7% [p = 0.046])
• Length of stay was reduced by 4.5 days
Age Ageing. 2007 Mar;36(2):190-6. Epub 2007 Jan 27.](https://image.slidesharecdn.com/thecomprehensivegeriatricassessment-pcpslides-211003083748/85/The-comprehensive-geriatric-assessment-pcp-slides-48-320.jpg)