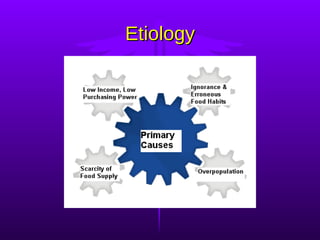
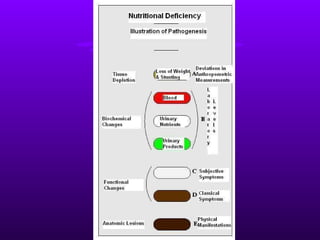
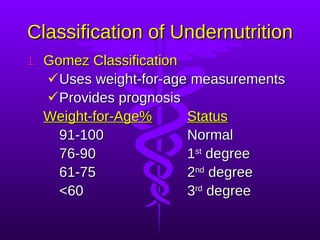
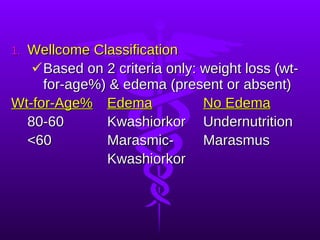
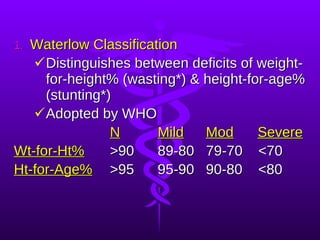
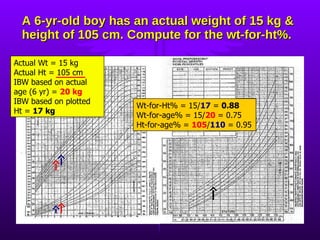
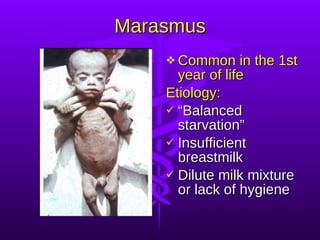
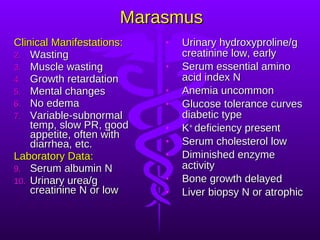
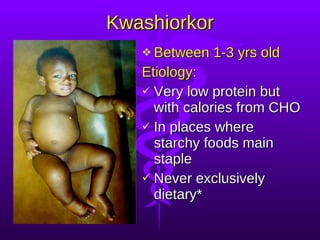
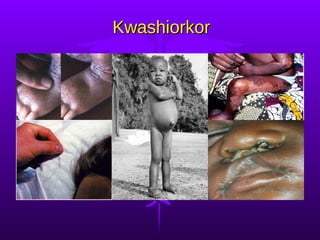
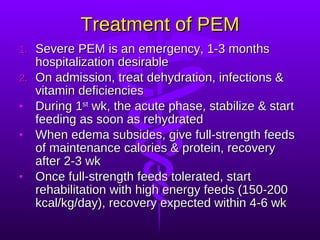
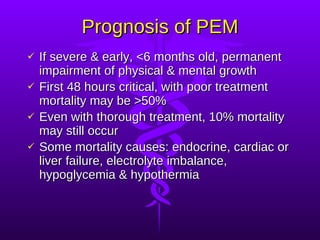
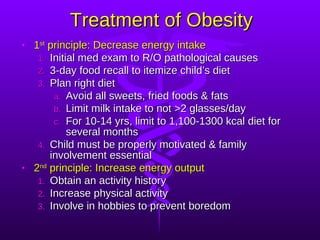
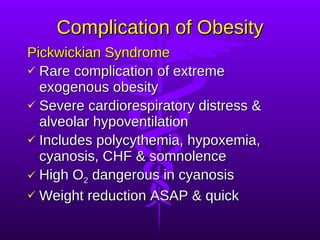
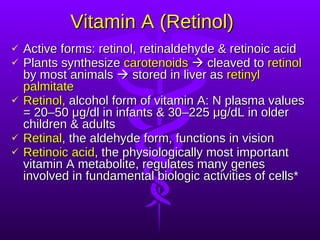
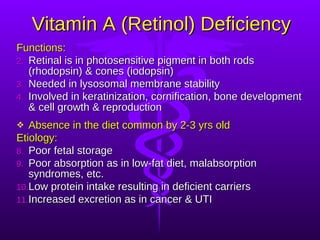
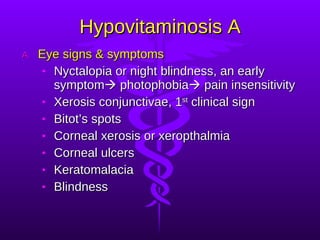
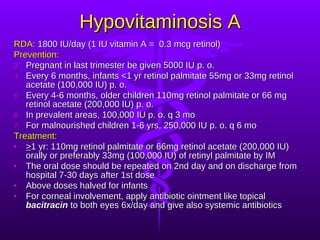
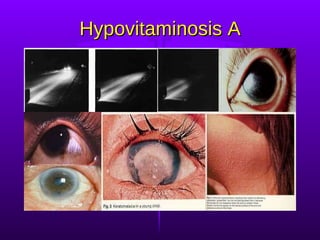
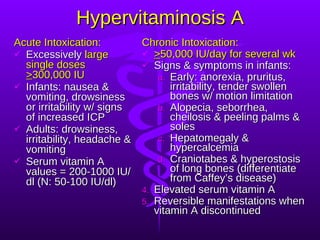
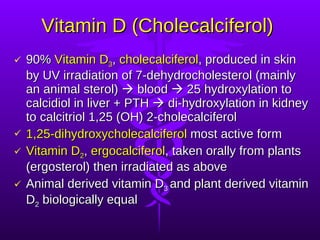
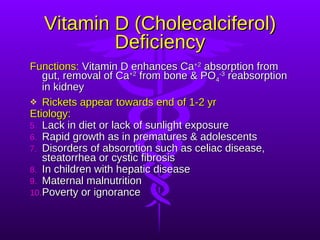
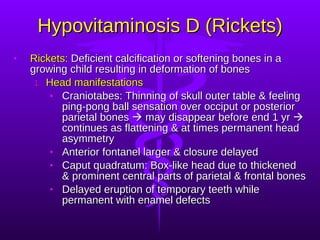
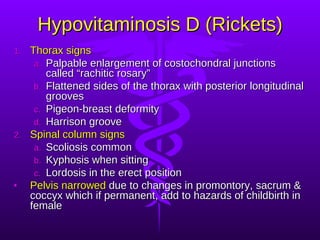
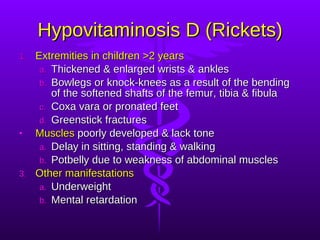
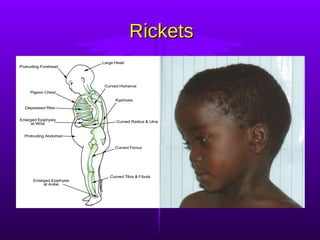
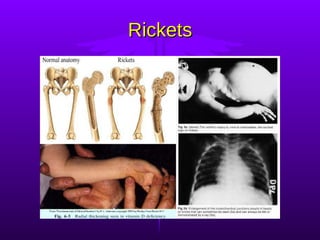
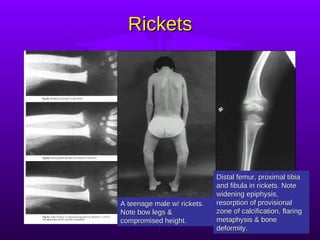
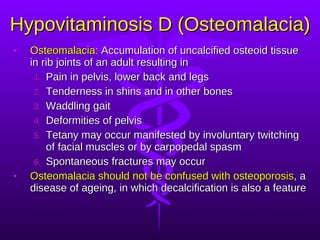
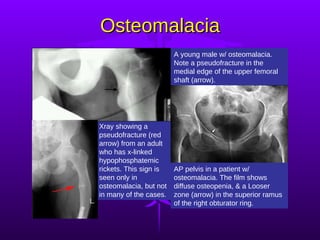
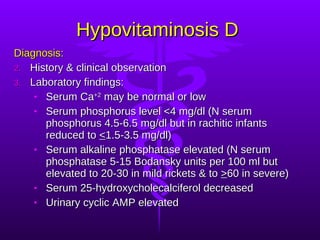
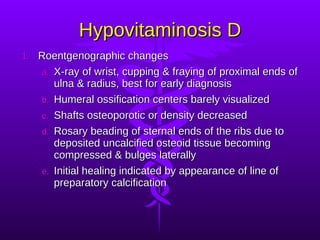
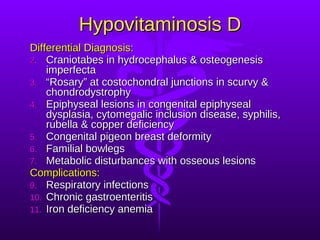
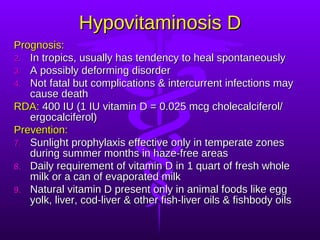
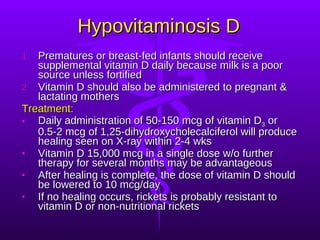
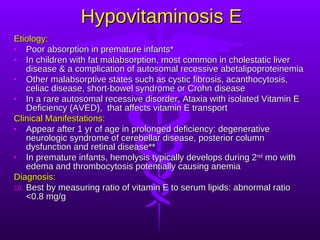
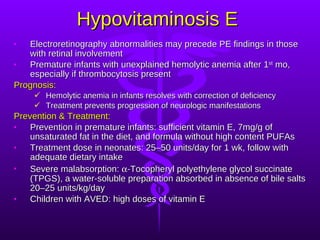
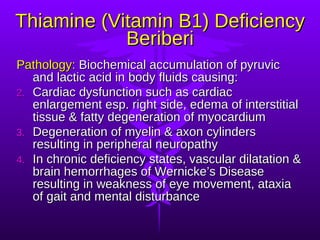
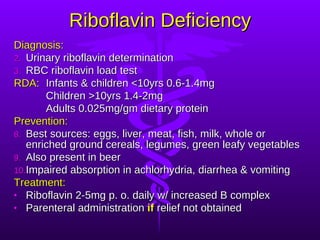
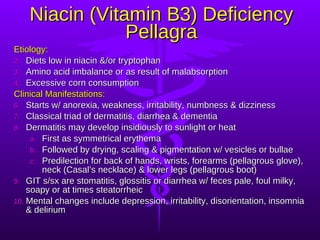
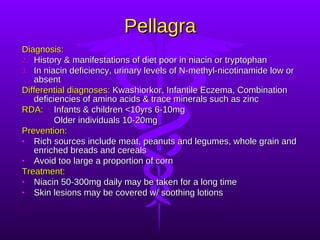
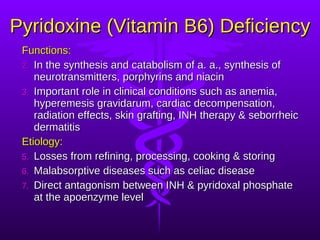
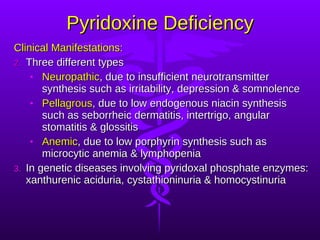
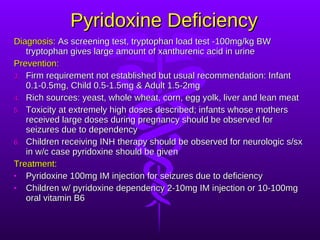
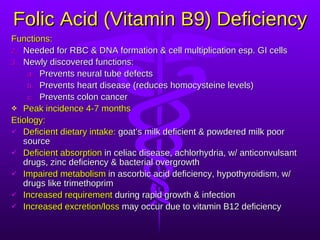
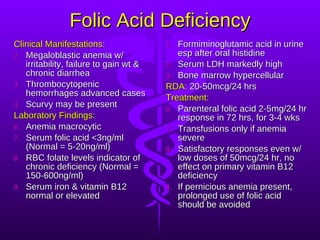
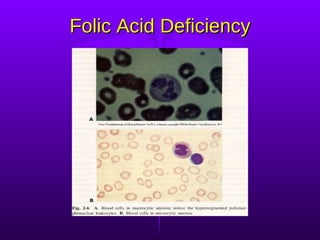
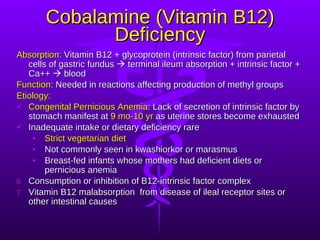
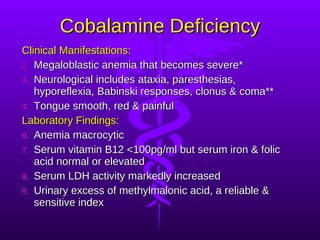
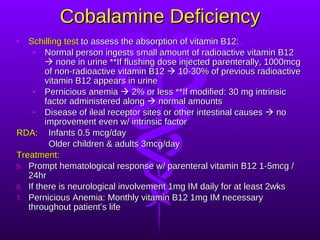
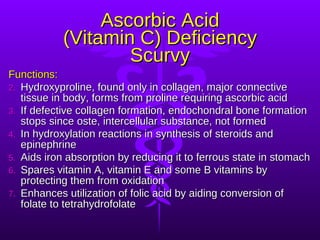
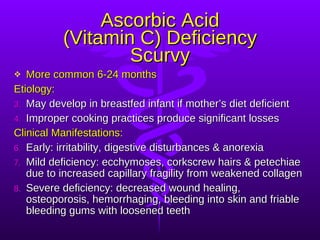
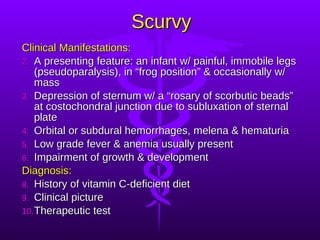
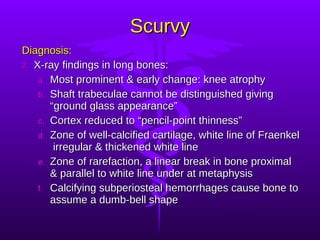
The document discusses various nutritional disorders including malnutrition, protein energy malnutrition (PEM), and specific vitamin deficiencies. It describes the classifications, etiologies, clinical manifestations, diagnoses, and treatments of marasmus, kwashiorkor, obesity, hypovitaminosis A, rickets, and osteomalacia. Key signs and laboratory findings for each condition are provided along with recommended daily allowances and prevention strategies.