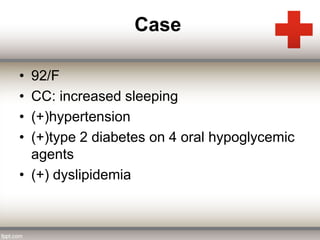
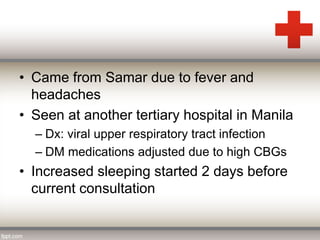
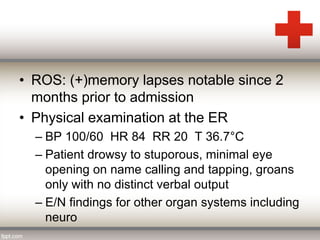
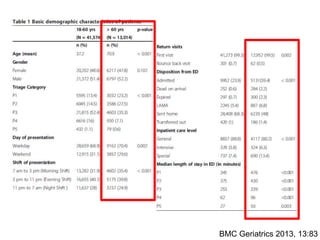
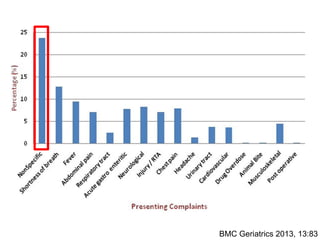
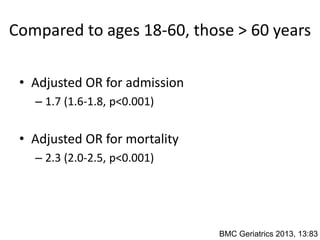
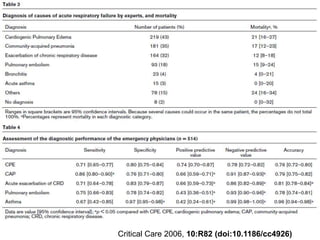
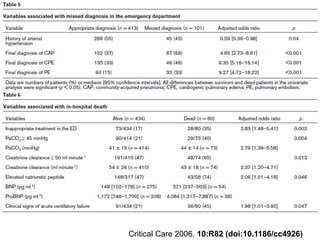
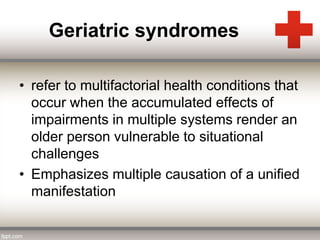
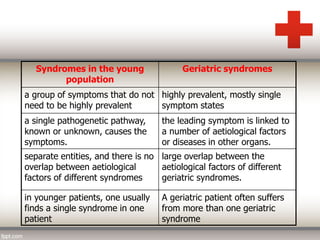
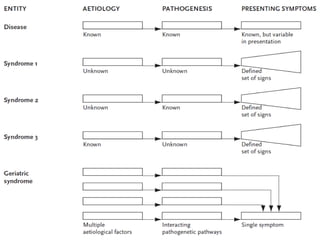
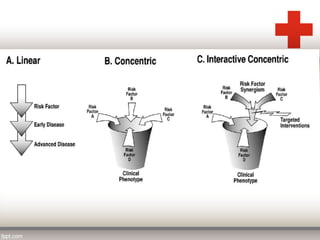
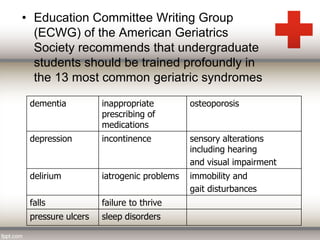
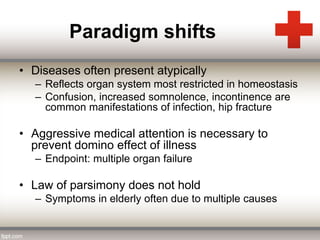
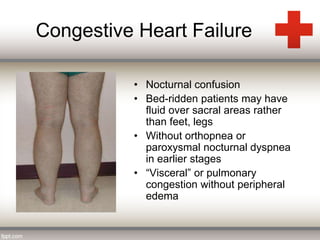
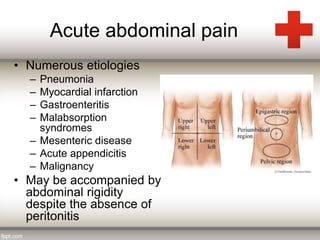
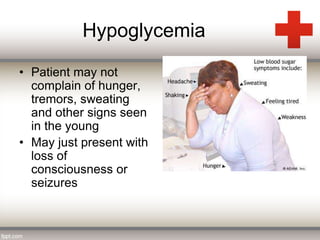
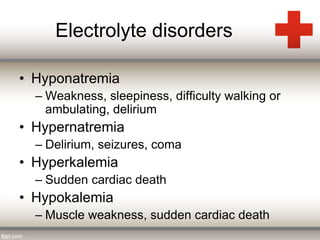
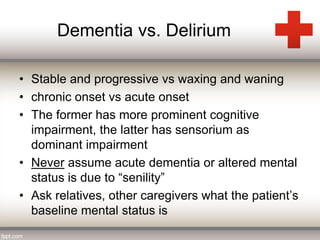
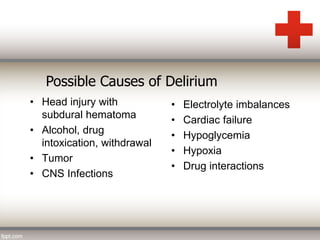
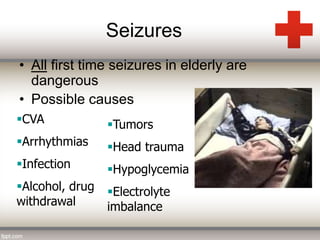
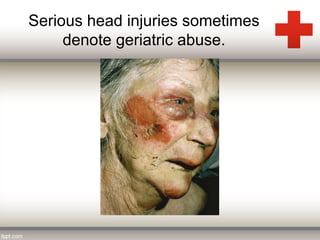
This document provides an overview of key considerations for emergency physicians in evaluating geriatric patients. It discusses how diseases often present atypically in older patients due to multiple organ system involvement. Common geriatric syndromes like falls, incontinence and delirium are described. The case study presented is of a 92-year-old woman who presents with increased sleeping; the initial impression is likely stroke or infection given her altered mental status and other chronic conditions. The document outlines the critical role of emergency physicians in caring for older patients and some common chief complaints like abdominal pain, confusion and electrolyte imbalances.