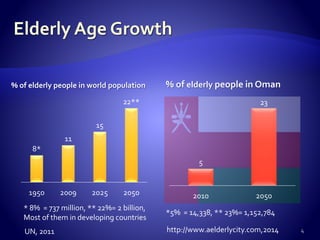
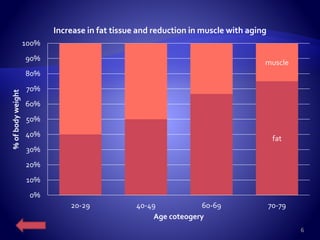
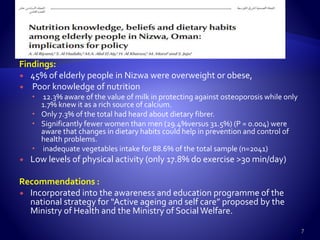
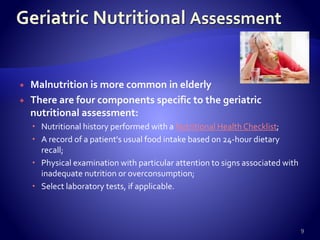
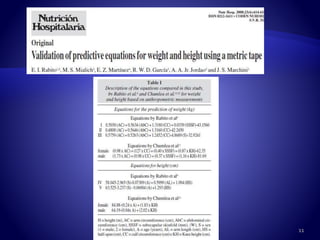
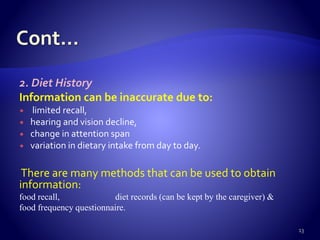
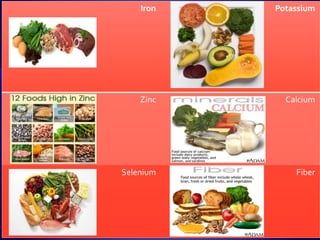
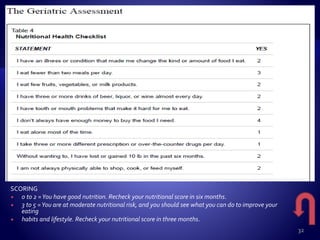
The document discusses the nutritional challenges faced by the elderly population, including age-related physiological changes, malnutrition prevalence, and the importance of proper dietary guidelines. It highlights the need for tailored nutritional interventions and physical activity to manage health in older adults and reduce risks associated with aging. Recommendations include monitoring dietary intake, encouraging hydration and physical activity, and addressing specific nutrient deficiencies such as vitamins B12 and D.