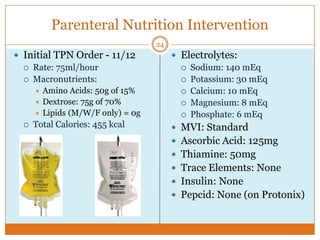
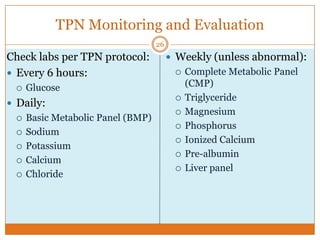
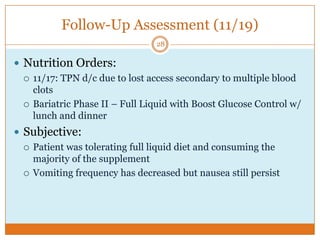
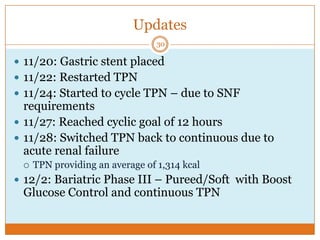
This document provides an overview of a 58-year-old female patient who underwent a sleeve gastrectomy surgery in July 2013 and experienced complications including a persistent gastric leak. It discusses her medical and surgical history, the nutrition care process being followed including assessments, diagnosis of altered GI function, interventions of initiating TPN and monitoring, and follow-up evaluations showing tolerance of TPN and a full liquid diet. The summaries provide the high-level details about the patient's history, surgery, complications, nutrition care and progress.