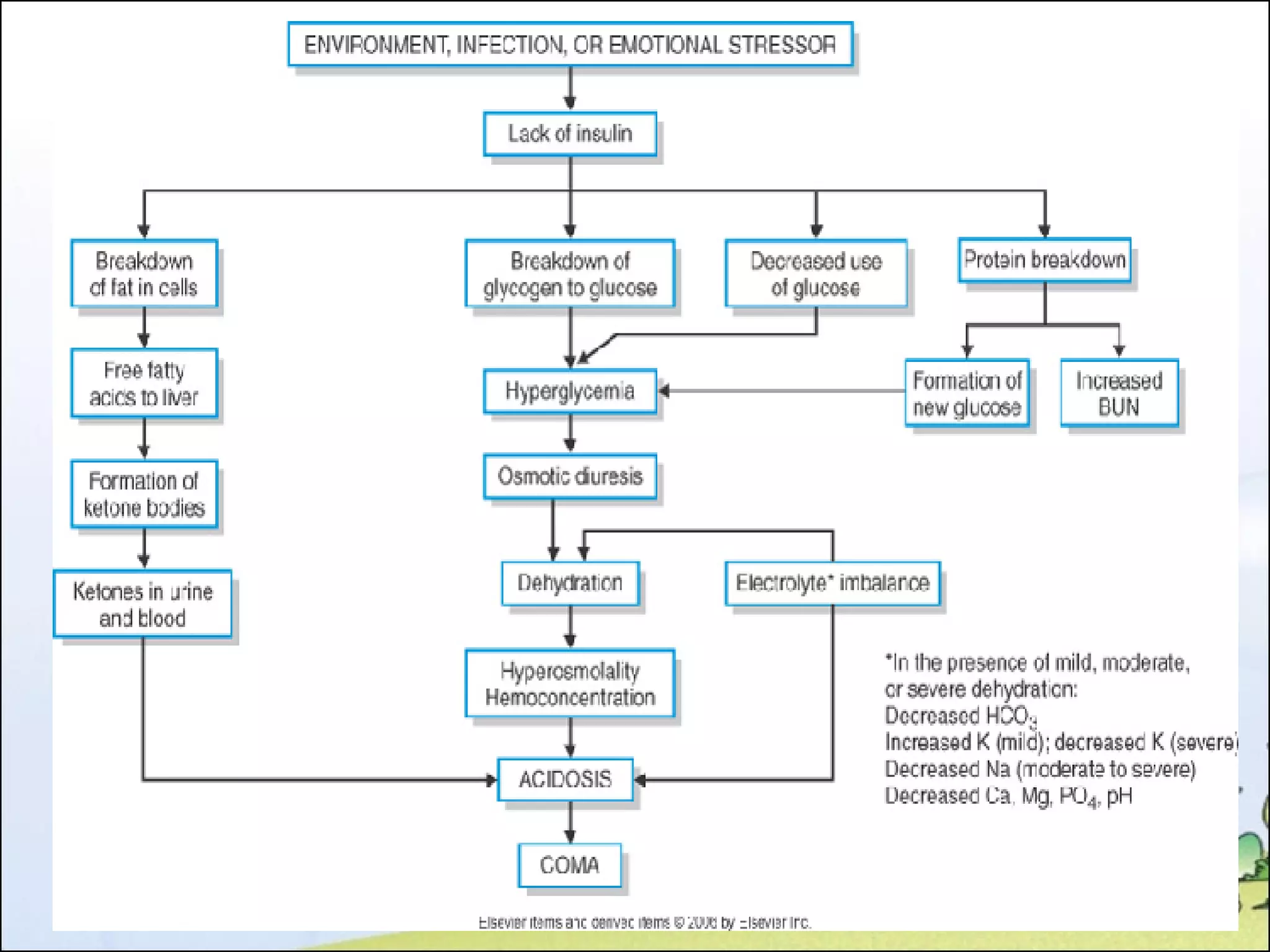
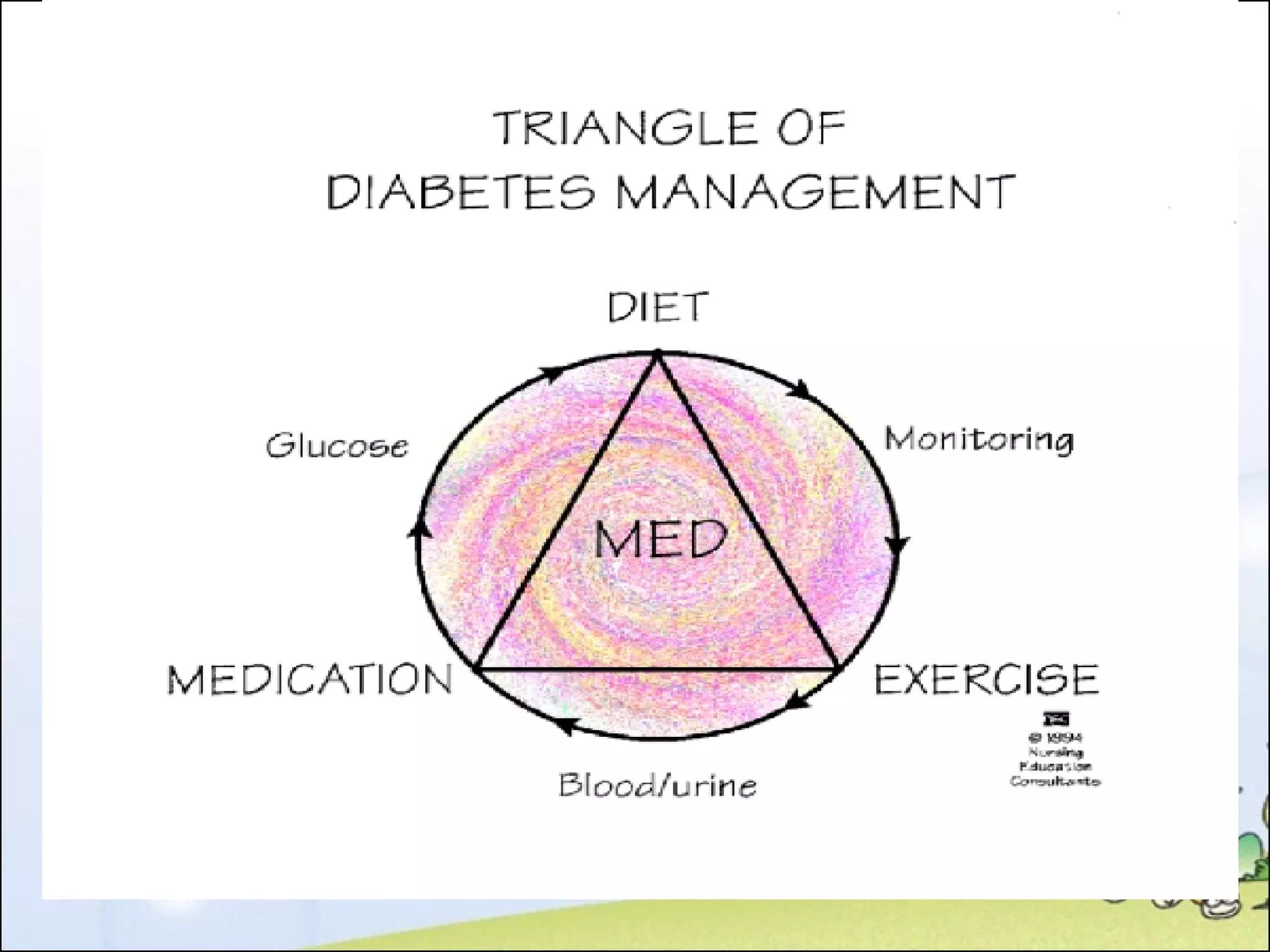
Diabetes mellitus is an endocrine disorder characterized by inadequate insulin production leading to hyperglycemia and its associated symptoms. It has two main types: Type 1 (insulin-dependent) and Type 2 (non-insulin-dependent), with various treatment options including dietary management, medications, and insulin therapy. Complications can arise from both hyperglycemia and hypoglycemia, necessitating careful monitoring and management to prevent severe outcomes.