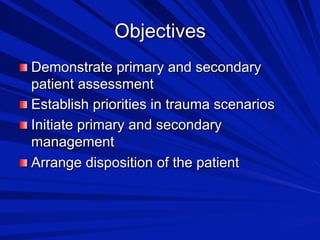
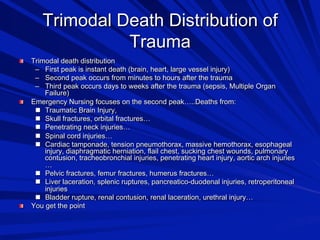
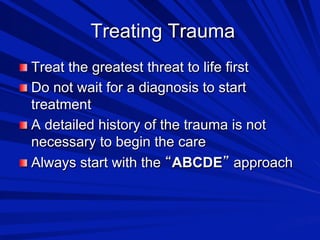
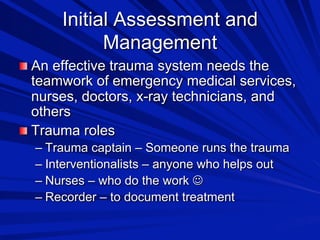
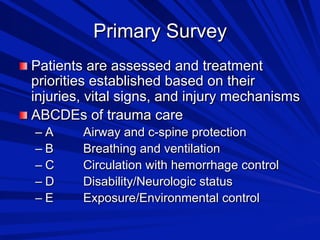
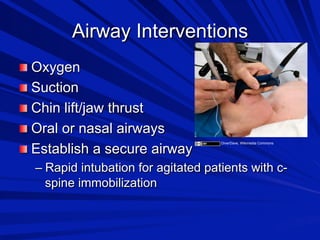
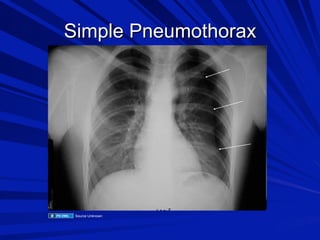
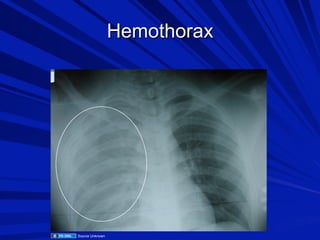
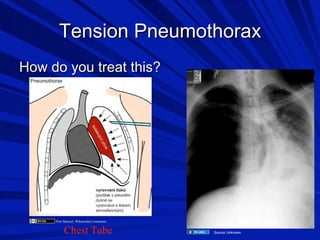
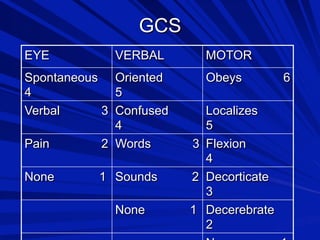
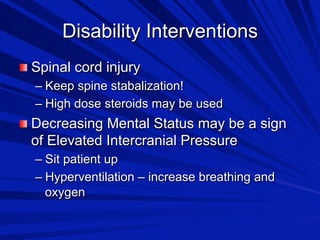
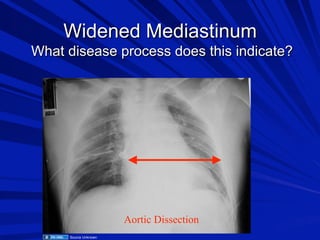
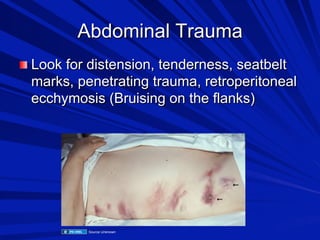
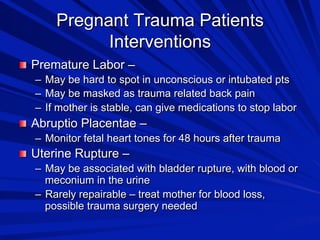
The document focuses on trauma assessment and management, detailing the importance of a systematic approach using the ABCDE method to prioritize patient care. It outlines various types of shock, assessment techniques, and interventions needed for different trauma scenarios, emphasizing teamwork among healthcare professionals. Key information on specific injuries, especially in pediatric and pregnant trauma patients, is discussed, highlighting the critical nature of timely interventions and ongoing assessments.