1. The primary survey in trauma management focuses on the ABCDE approach to identify and treat life-threatening injuries. This includes assessing the airway, breathing, circulation, disability, and exposure.
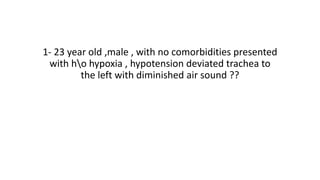
2. Maintaining an open airway is critical and may require techniques like head tilt/chin lift or jaw thrust. Oropharyngeal or nasopharyngeal airways can be used if needed. Tension pneumothorax requires urgent needle decompression and chest drain placement.
3. In addition to airway management, the primary survey involves evaluating breathing/ventilation and looking for signs of respiratory distress or reduced breath sounds. Circulation is also assessed to control hemorrhage and ensure adequate end-organ