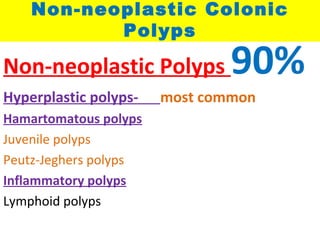
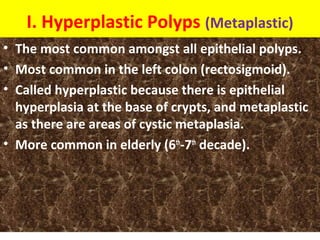
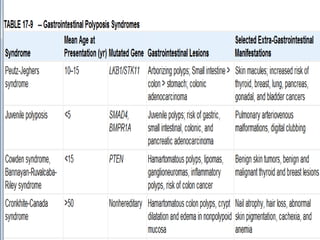
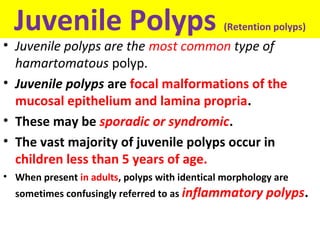
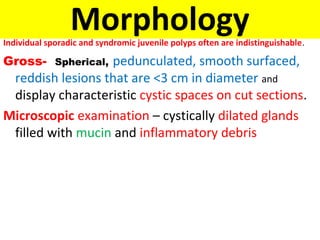
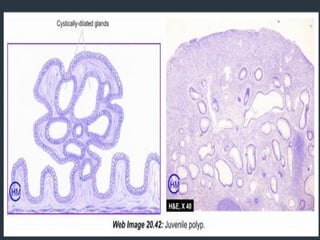
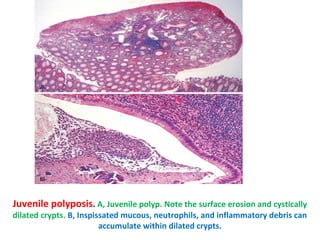
Non-neoplastic colonic polyps are very common growths in the large intestine. The majority are non-neoplastic polyps, with hyperplastic polyps being the most common type. Other non-neoplastic polyp types include hamartomatous polyps, such as juvenile polyps and Peutz-Jeghers polyps, as well as inflammatory polyps. These polyps are generally not cancerous but in some rare syndromes they may have a small risk of becoming cancerous over time.