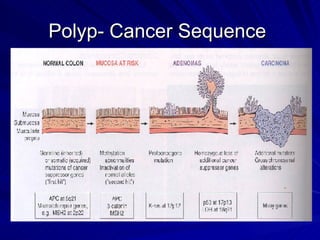
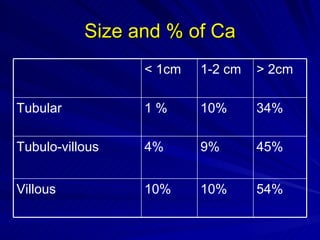
1) Colonic polyps can be neoplastic or non-neoplastic, with adenomatous polyps being precursors for colon cancer. Larger and villous polyps carry higher cancer risk.
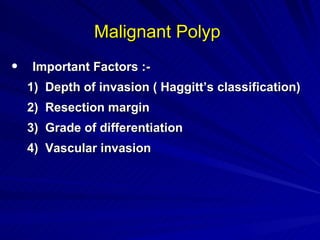
2) Management of polyps depends on size, histology, and risk factors. Low-risk polyps can be removed endoscopically, while malignant or high-risk polyps may require surgery based on factors like margins, invasion, and differentiation.
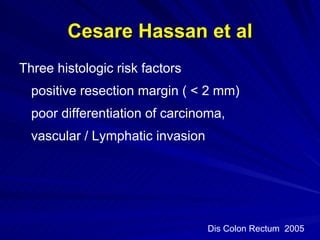
3) Studies have shown poor differentiation, vascular/lymphatic invasion, and margins less than 2mm to be histologic risk factors associated with residual disease and poorer outcomes, necessitating surgery for high-risk malignant polyps.