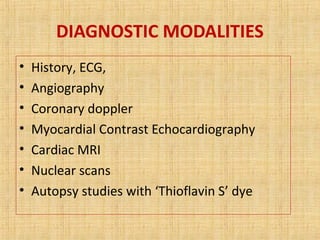
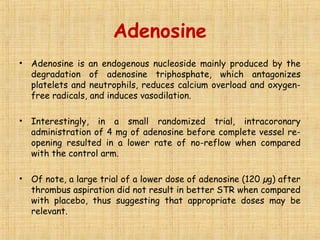
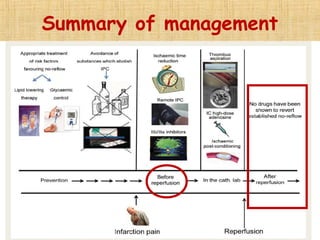
This document discusses the no-reflow phenomenon, which occurs when restoration of coronary artery patency after procedures like primary percutaneous coronary intervention (PCI) does not translate to improved tissue perfusion. No-reflow occurs in 30% of patients after reperfusion for acute myocardial infarction and is associated with worse outcomes. It is caused by microvascular obstruction from distal embolization, ischemic injury, reperfusion injury, and individual patient susceptibility. Methods to diagnose no-reflow include angiography, coronary Doppler, cardiac MRI, and myocardial contrast echocardiography. Prevention strategies target reducing ischemic time, microvascular spasm, and distal embolization through early reperfusion, pharmacological agents, and ischemic conditioning techniques.