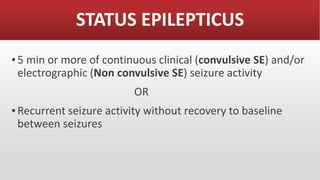
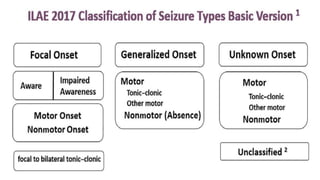
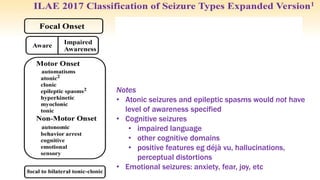
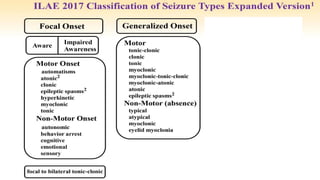
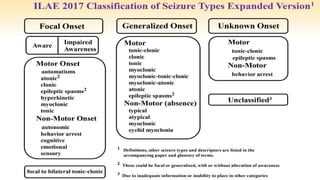
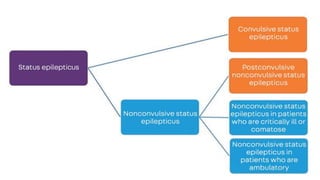
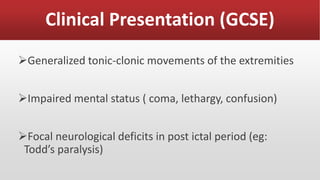
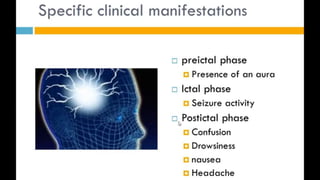
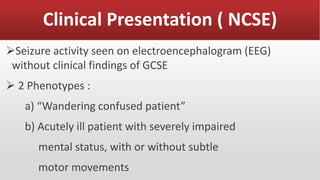
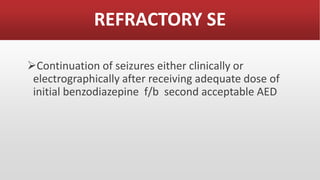
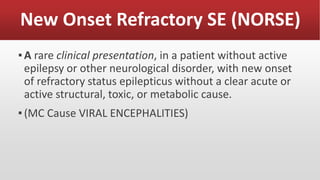
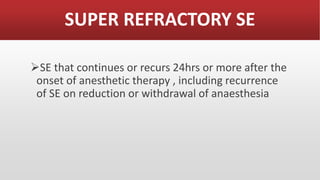
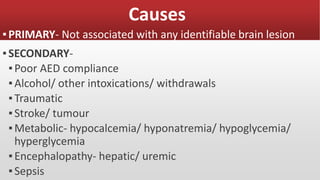
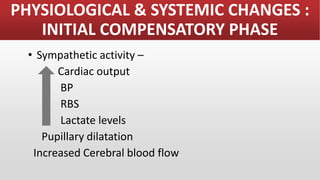
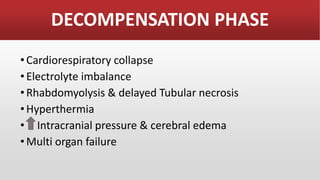
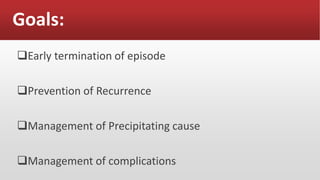
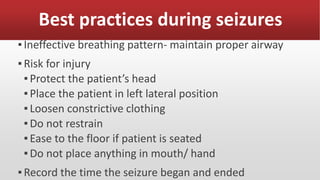
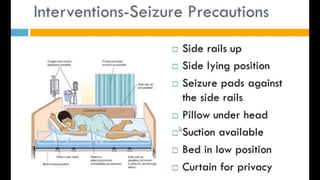
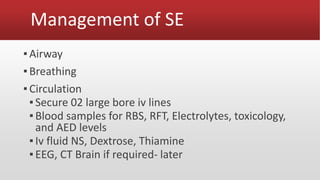
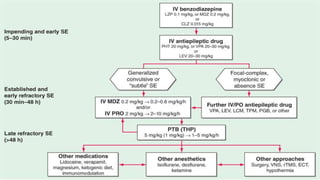
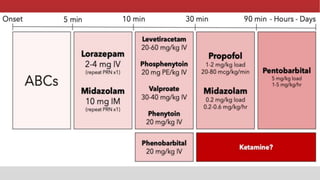
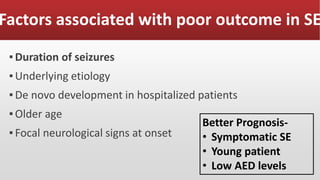
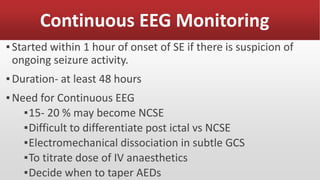
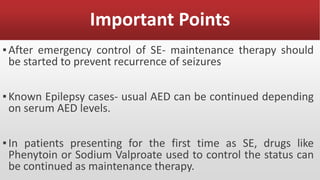
This document discusses the management of status epilepticus. It defines status epilepticus as continuous seizure activity lasting 5 minutes or more, or recurrent seizures without recovery between seizures. Status epilepticus is a medical emergency that can cause neuronal injury if not treated quickly. The document outlines the clinical presentations, causes, goals of management, and factors associated with poor outcomes of status epilepticus. It also discusses the treatment approach, including airway management, medications, continuous EEG monitoring, and importance of preventing recurrence.