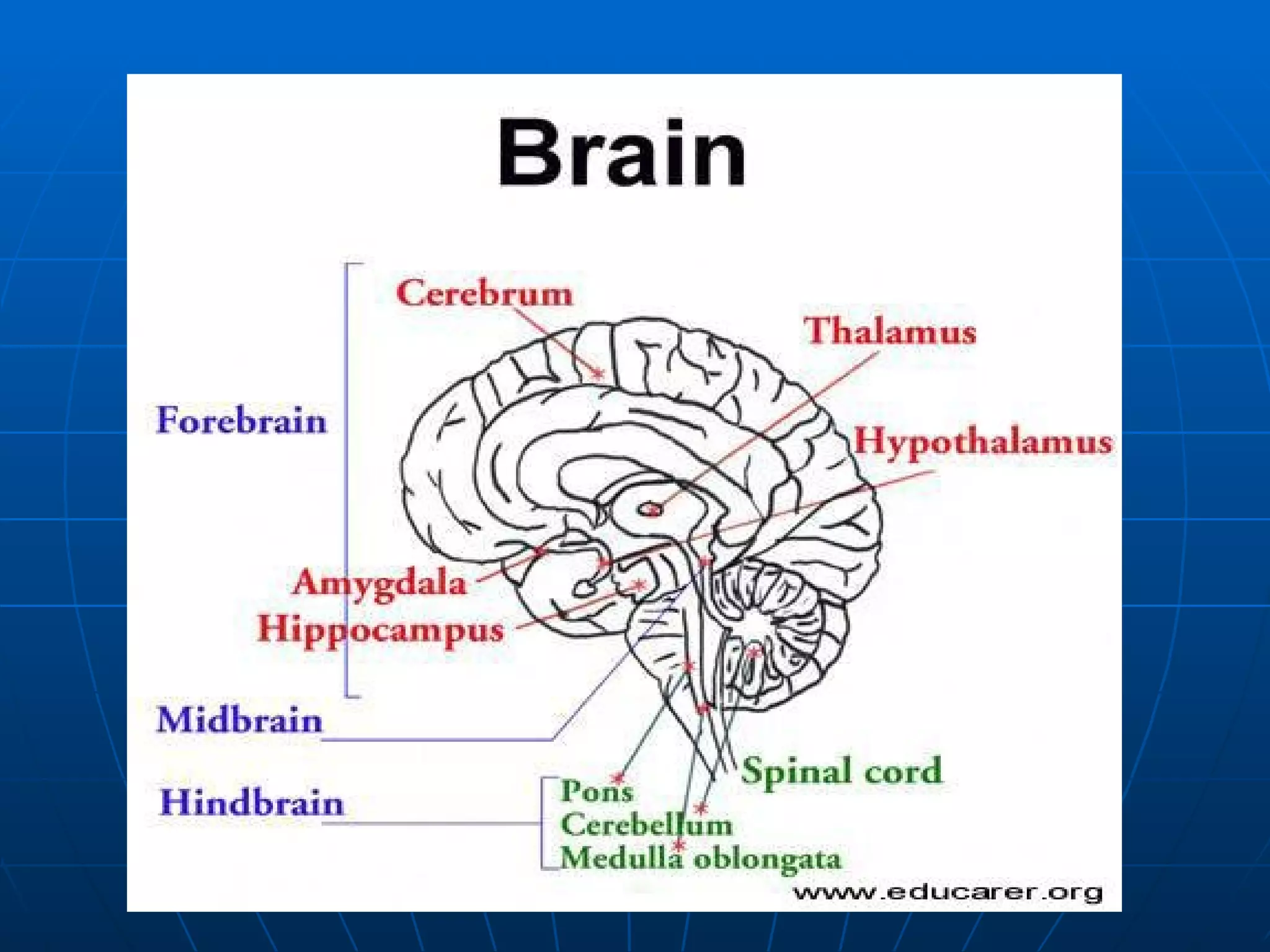
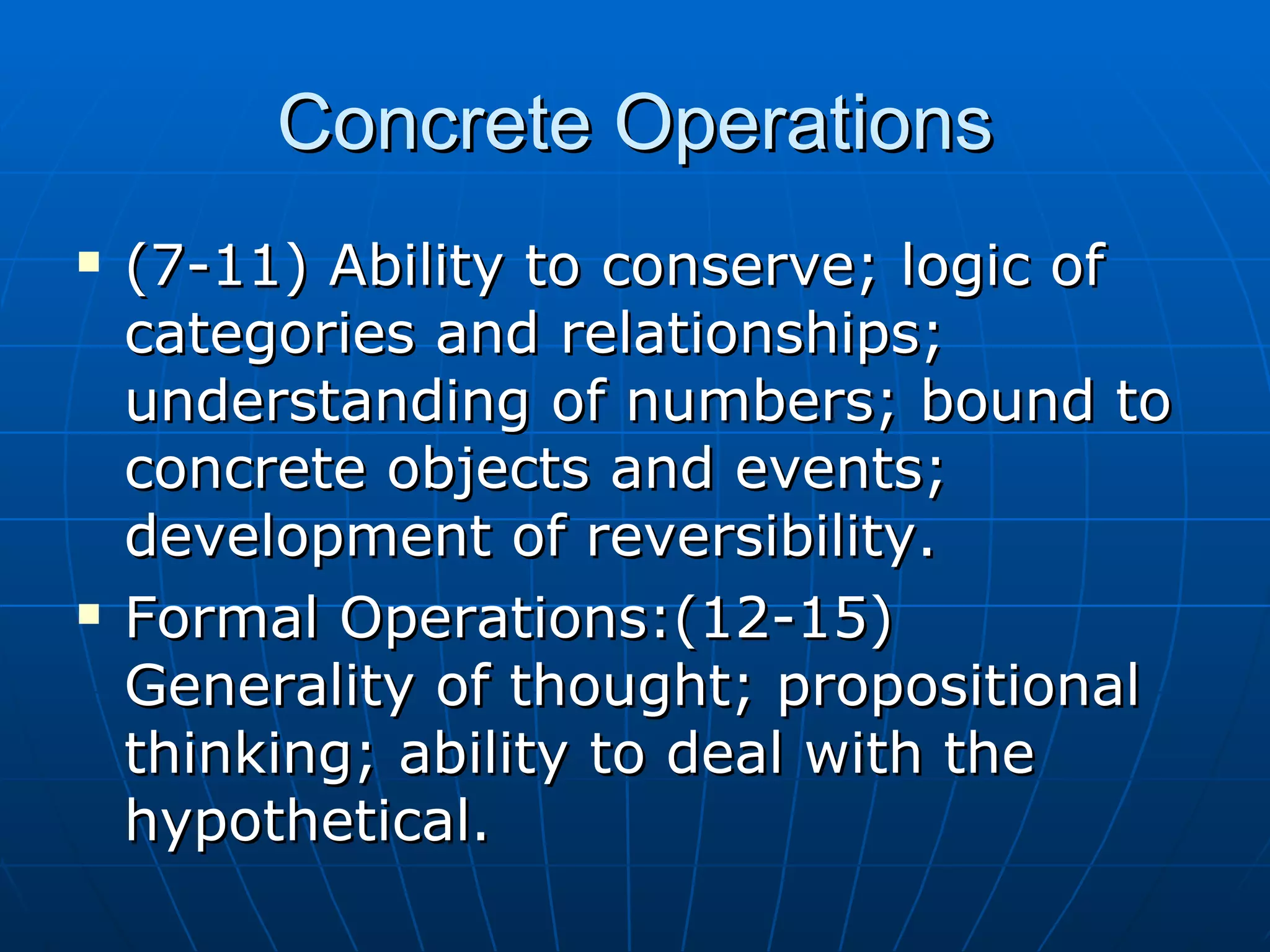
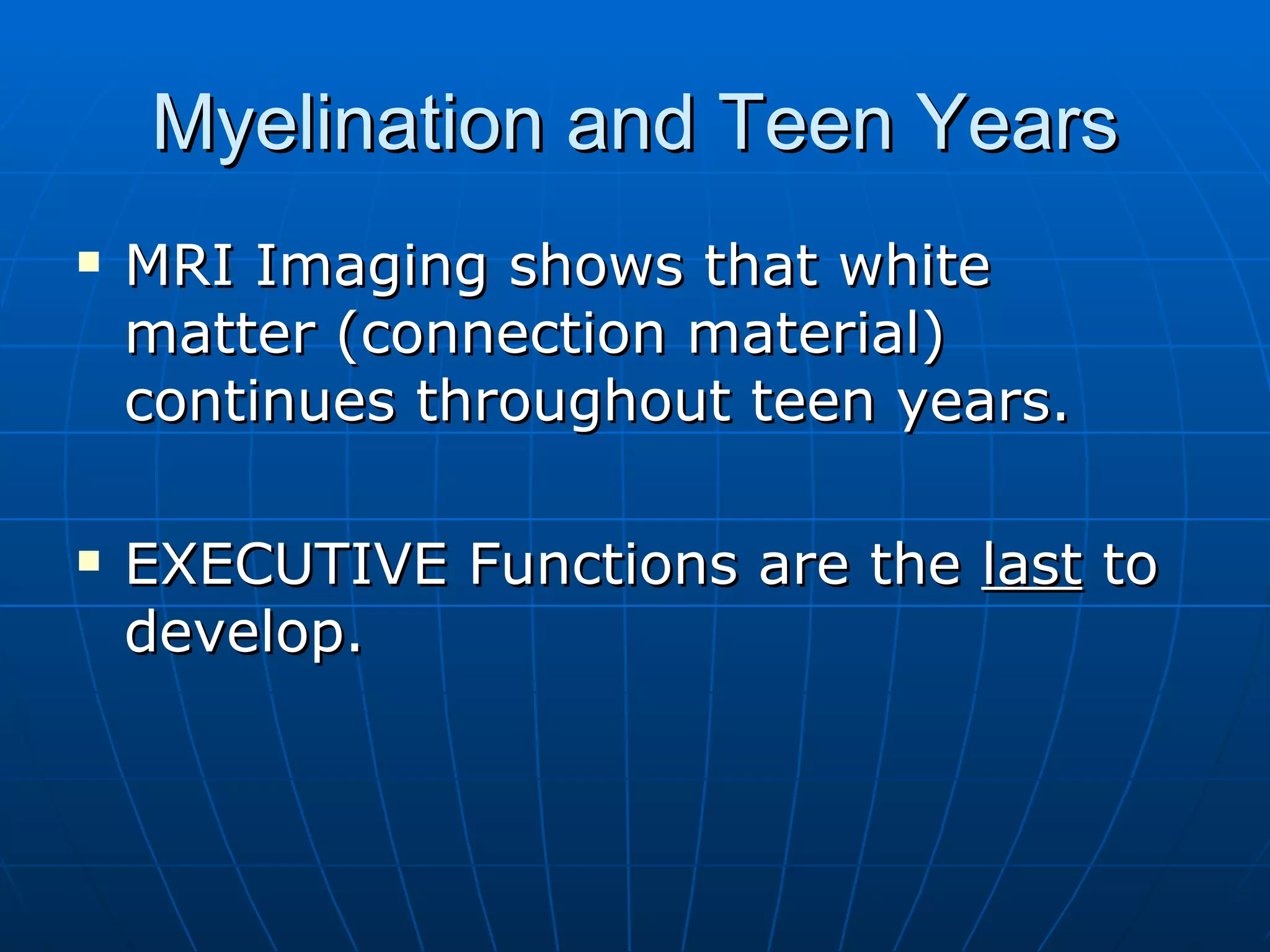
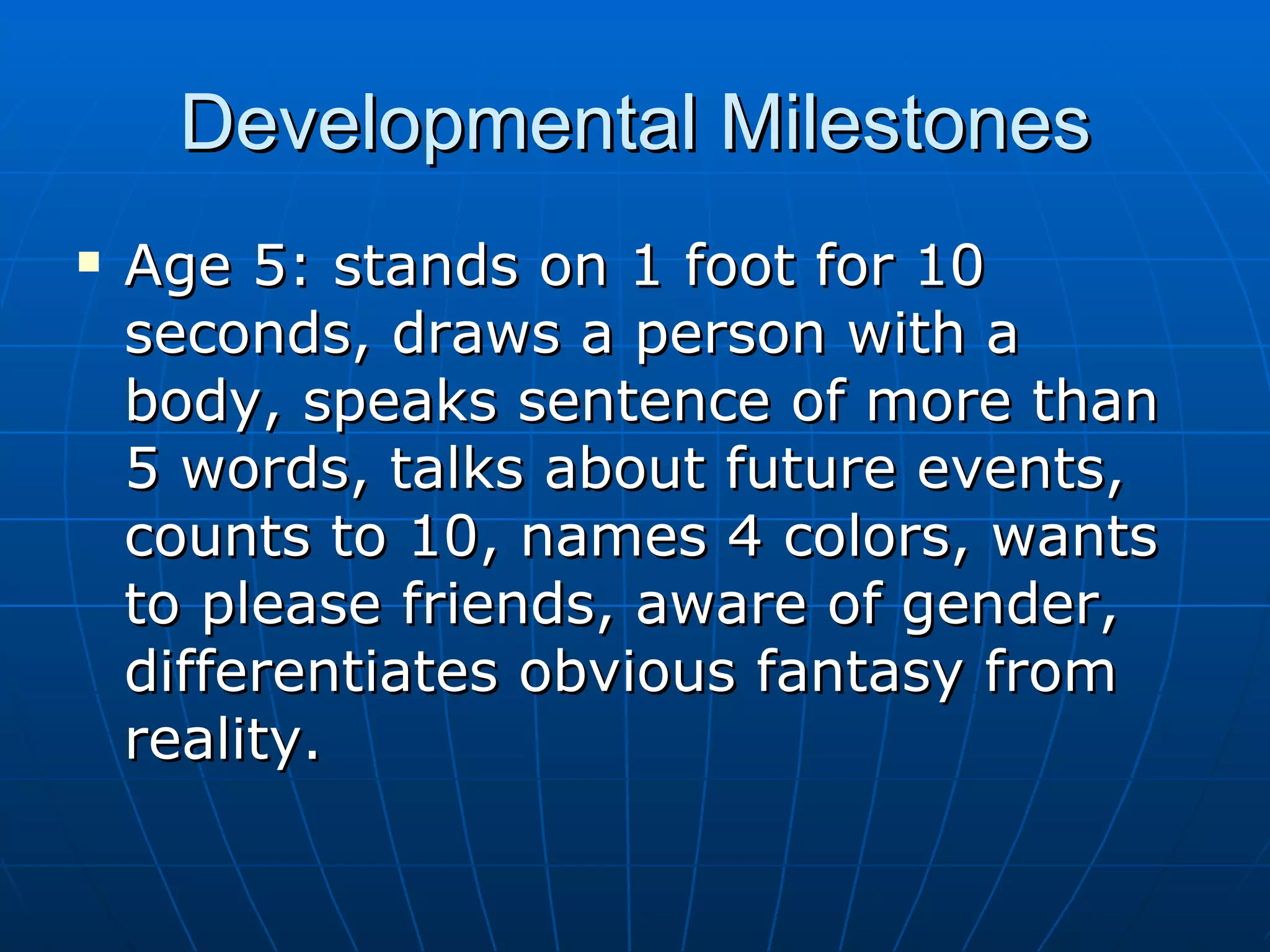
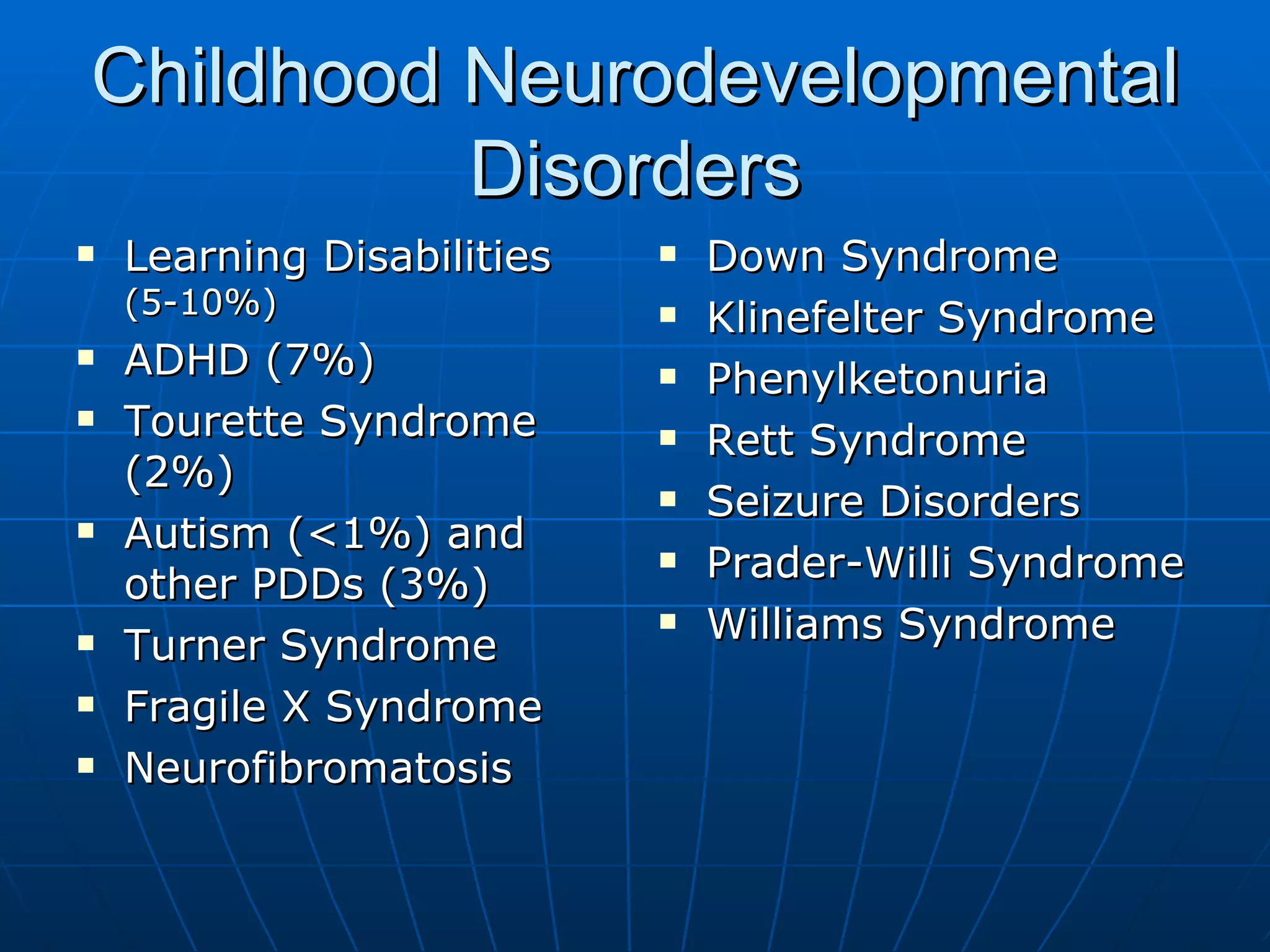
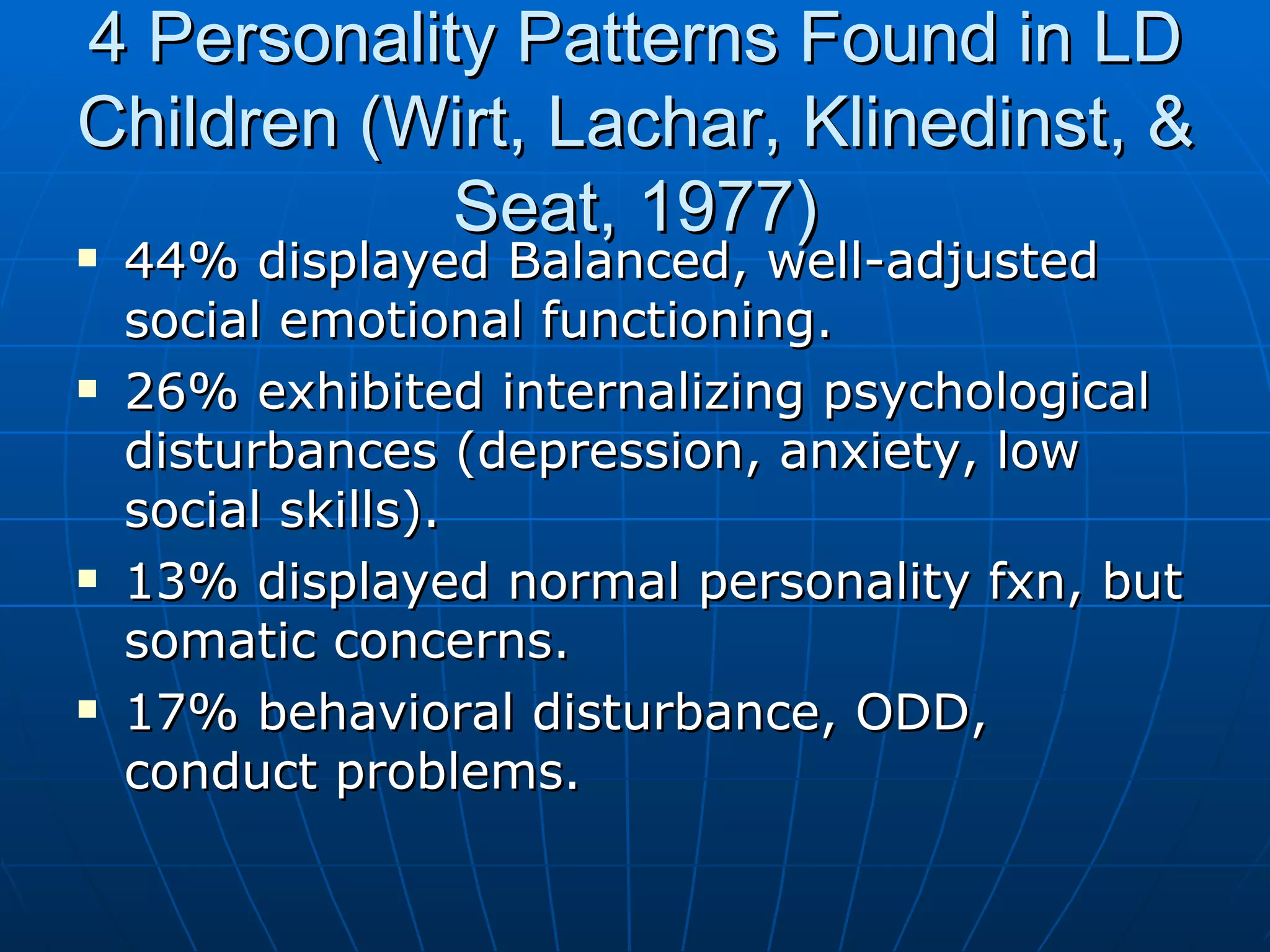
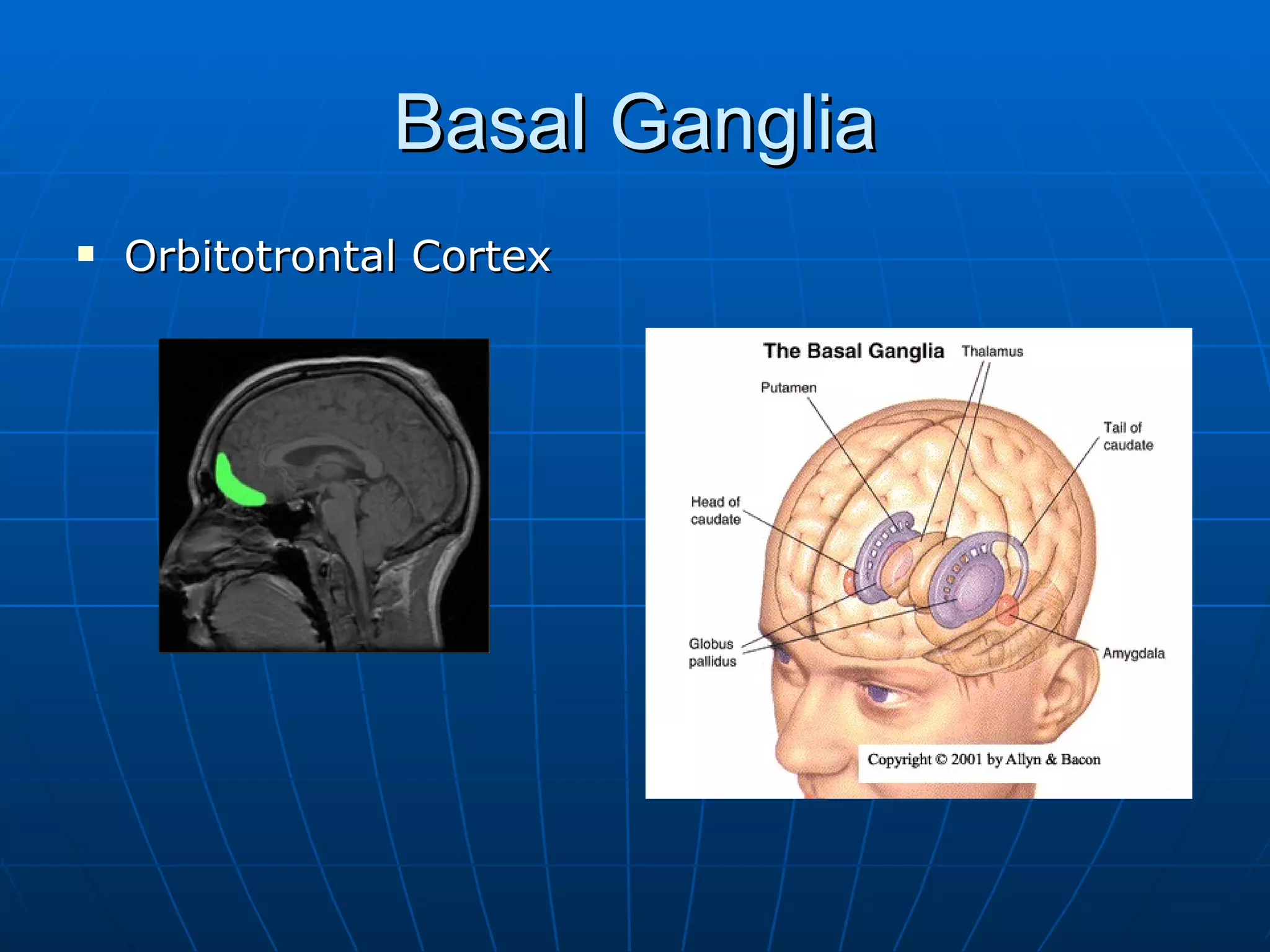
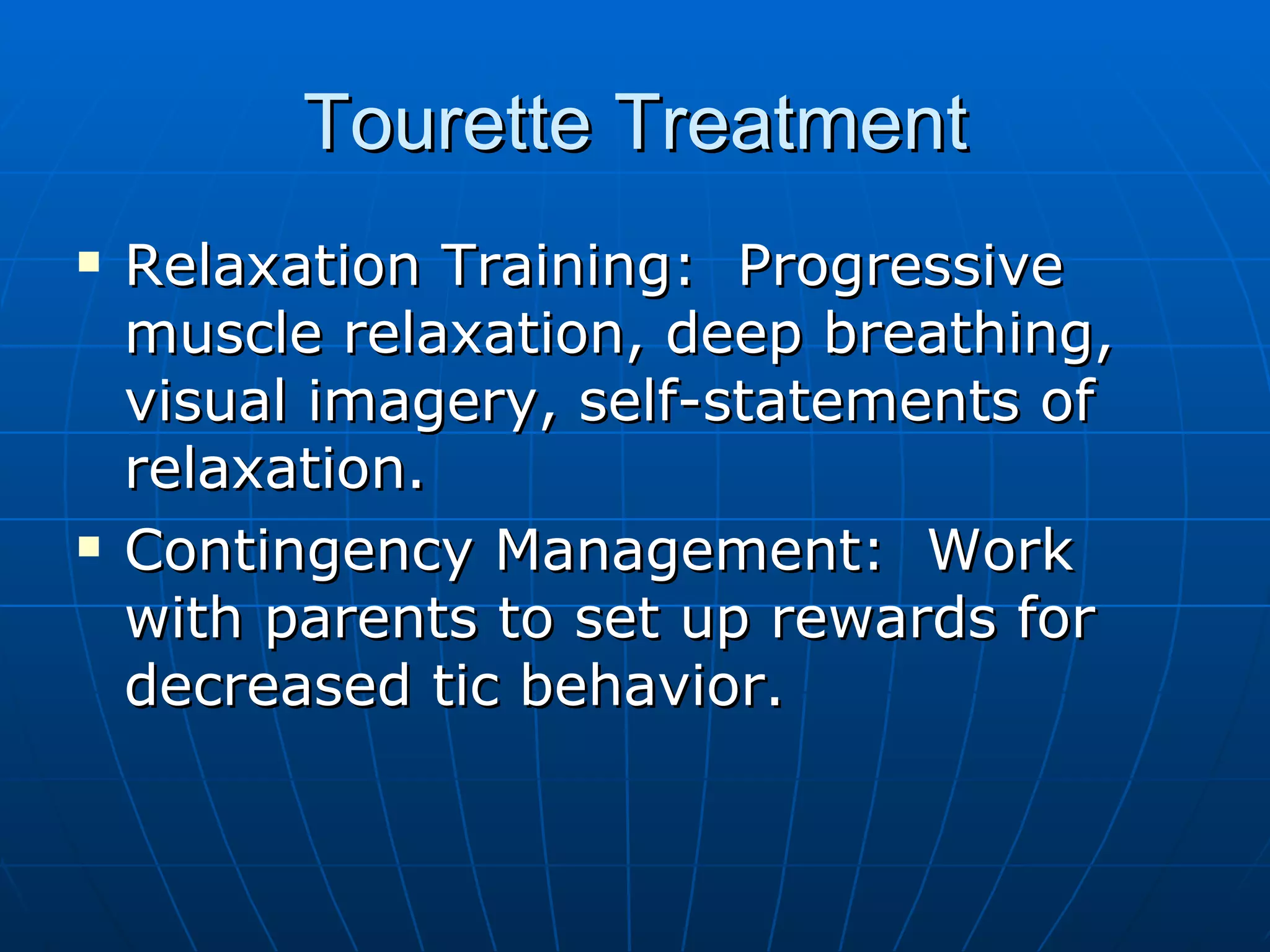
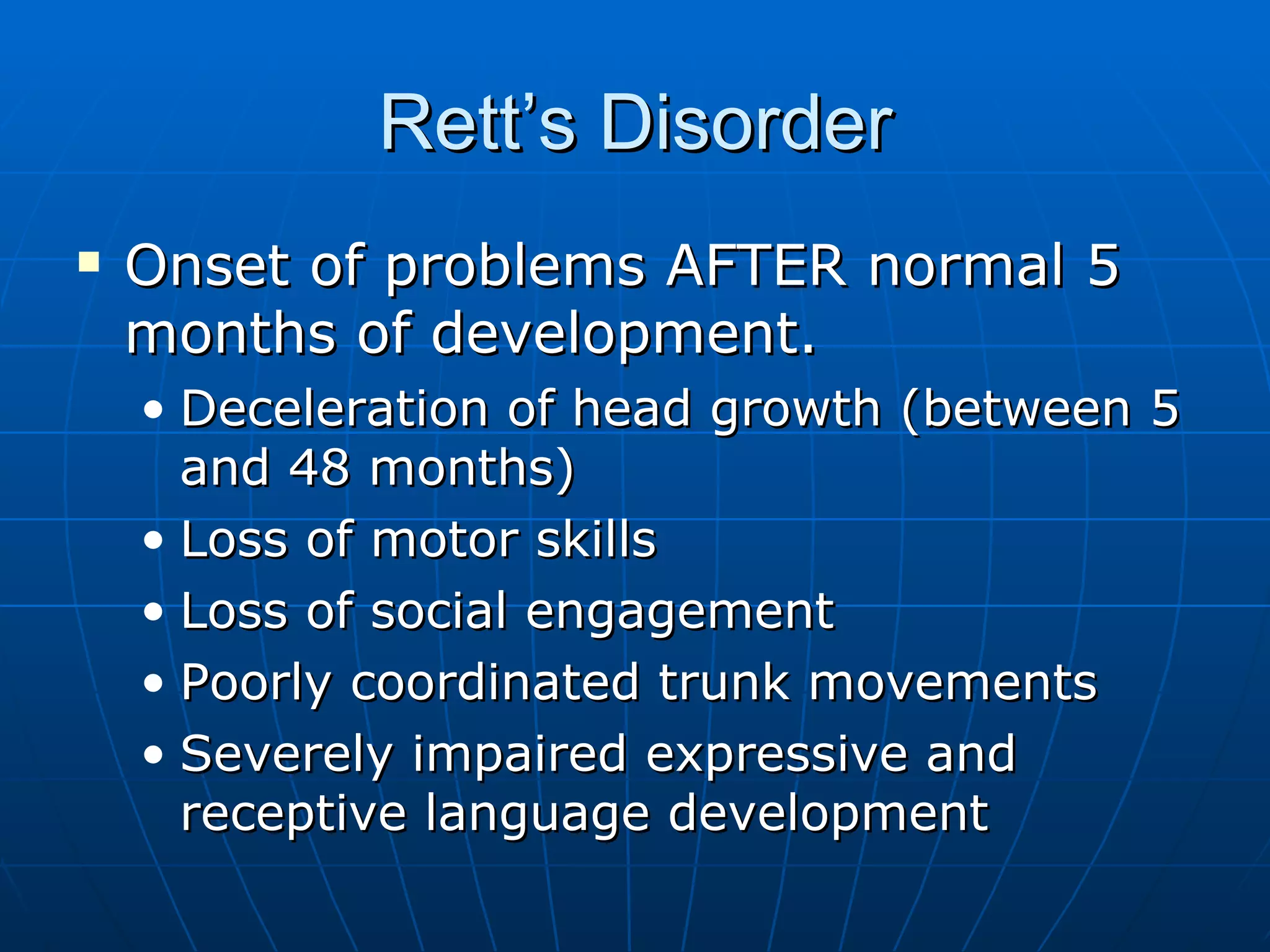
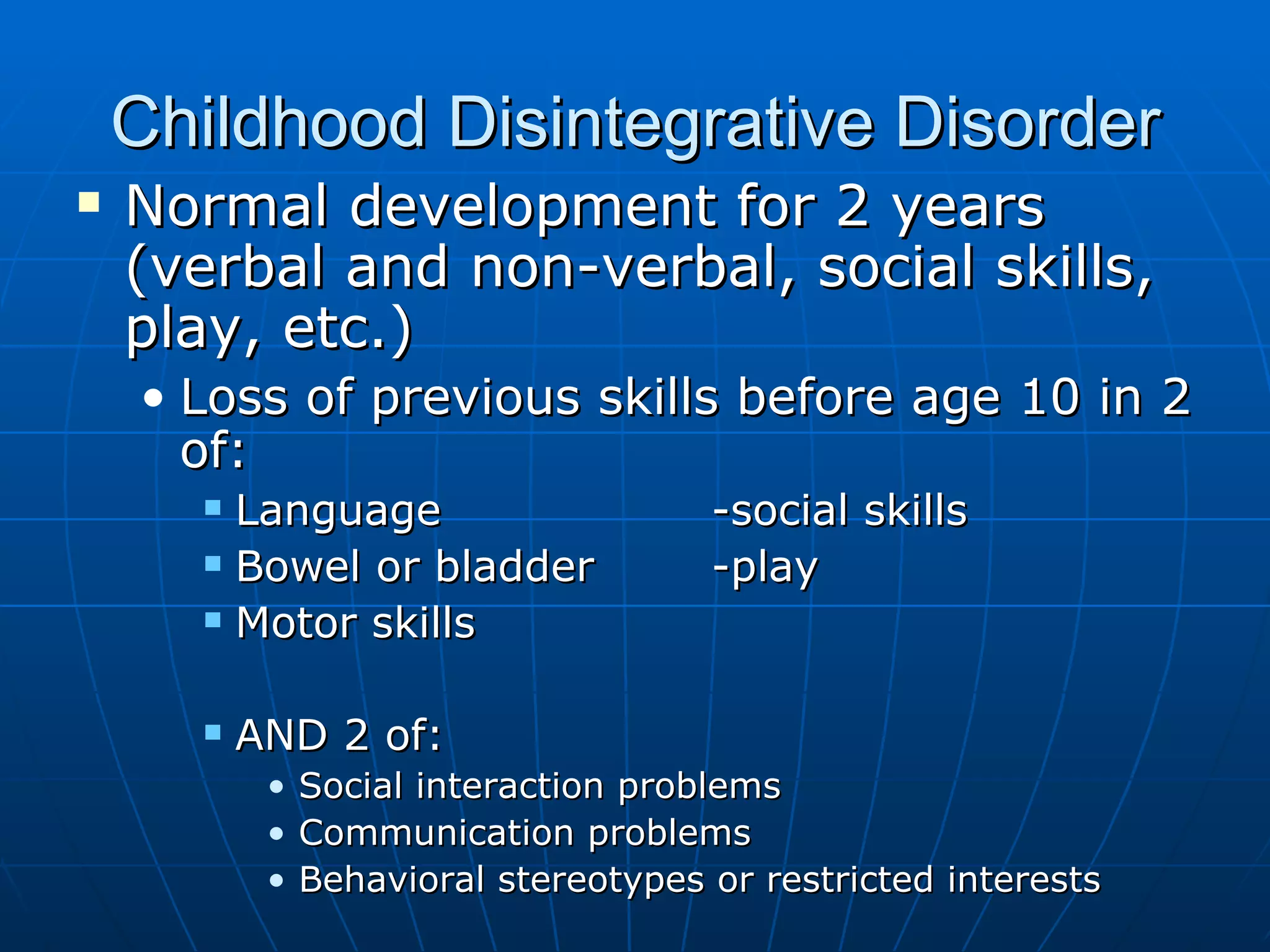
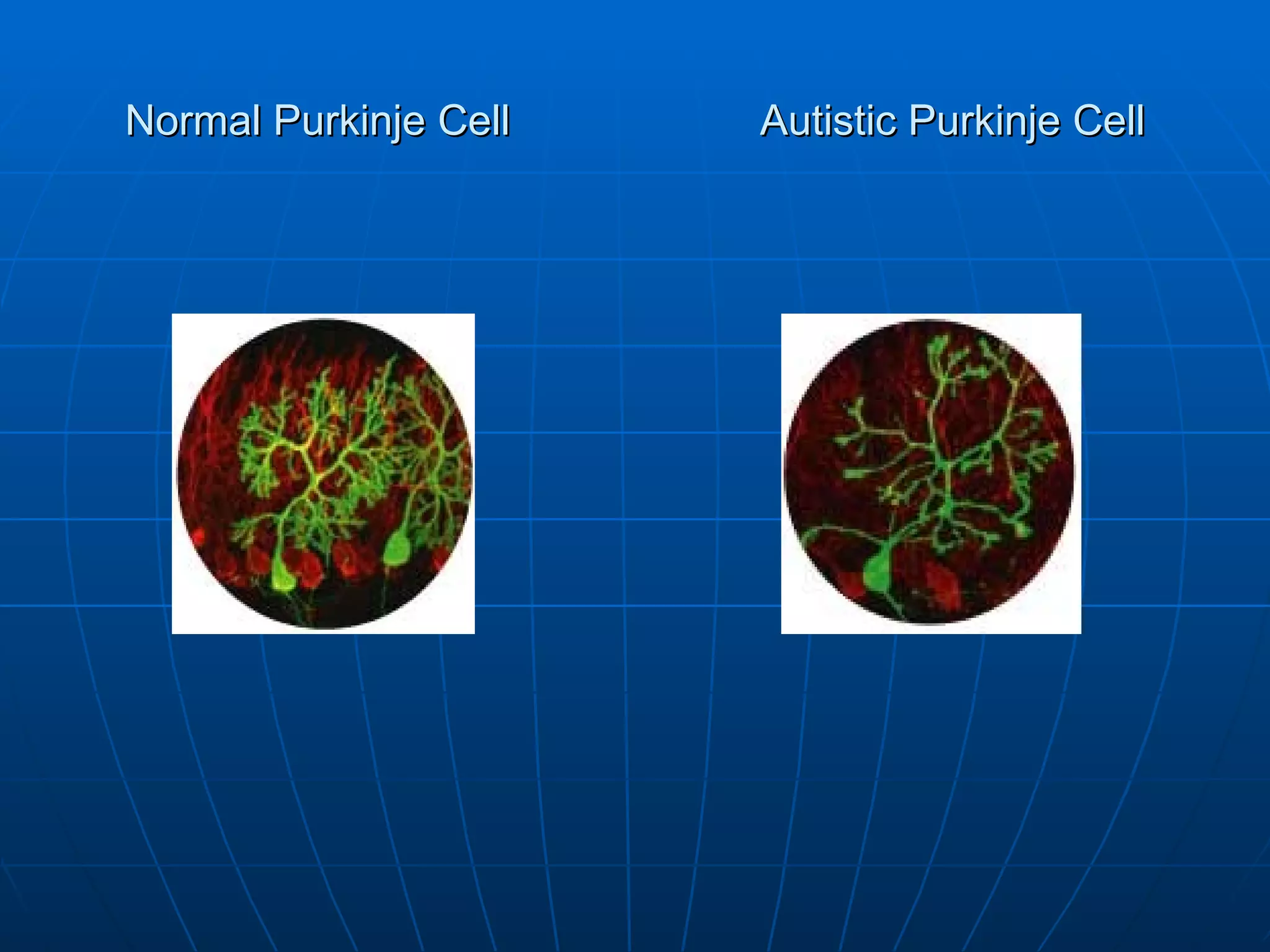
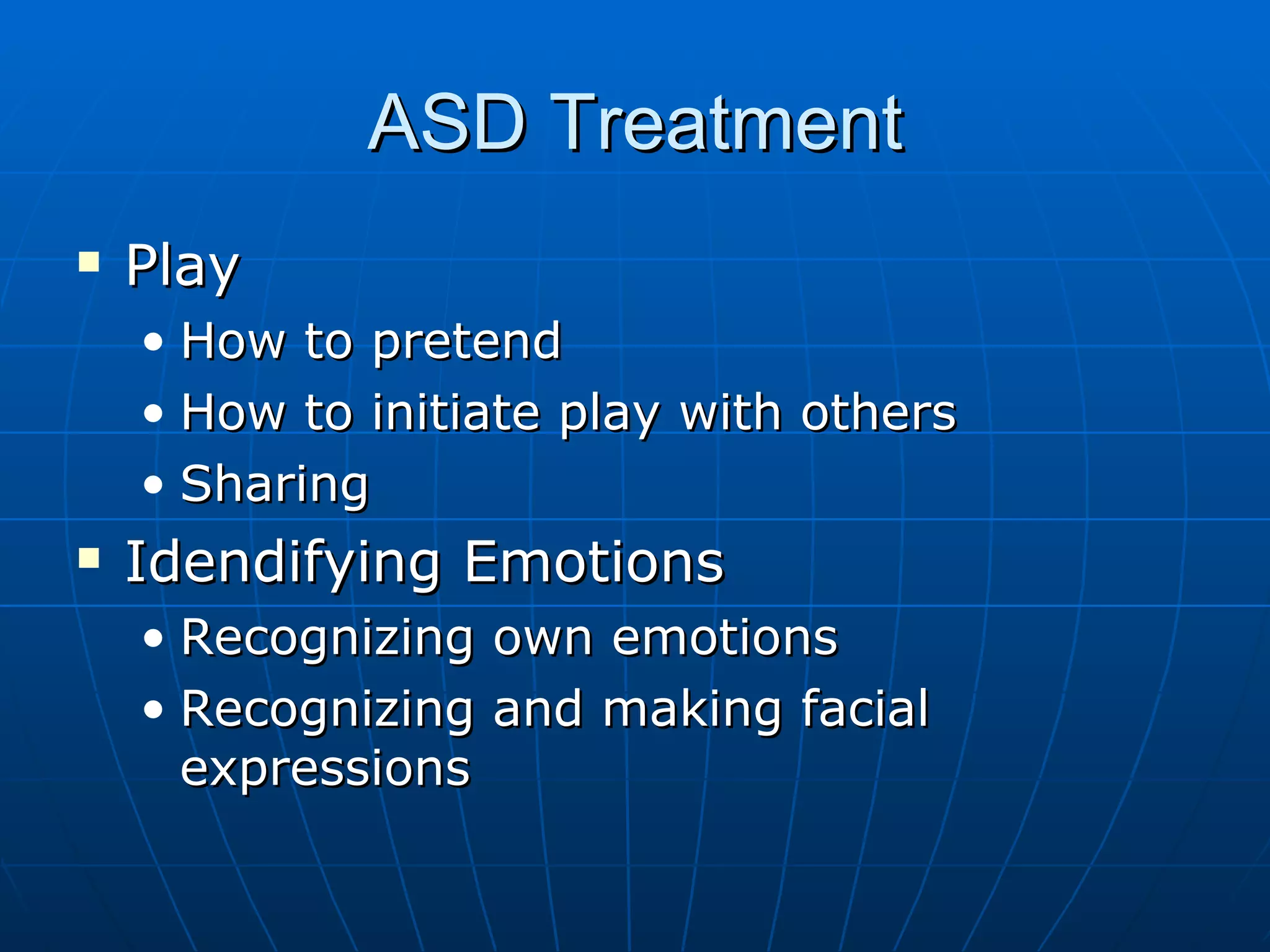
This document summarizes key aspects of neuropsychological development from infancy through adolescence, including major developmental milestones, disorders, and treatment approaches. It discusses phases of brain development, Piaget's stages of cognitive development, myelination and executive function development through the teen years. Common childhood neurodevelopmental disorders like learning disabilities, ADHD, autism, and Tourette's syndrome are described. Treatment approaches for these disorders focus on behavioral, educational, social skills, and medical interventions.