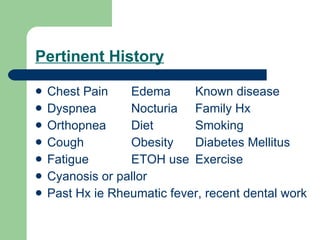
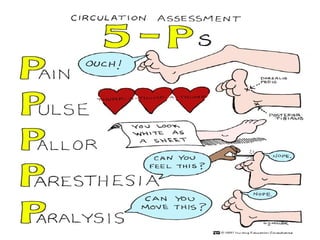
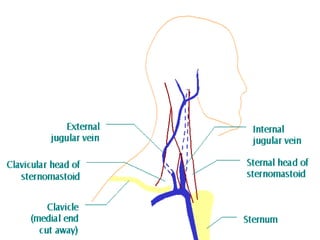
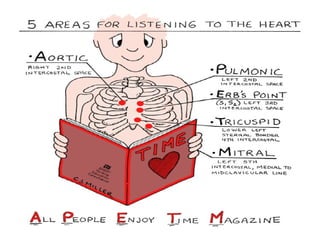
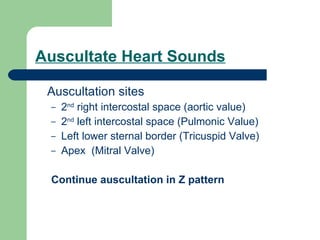
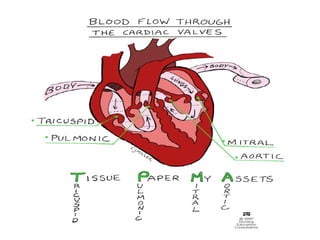
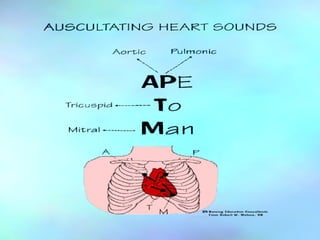
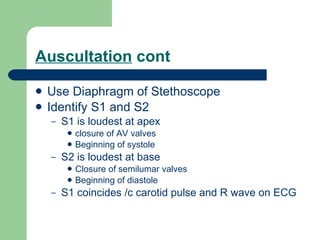
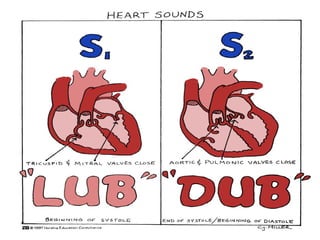
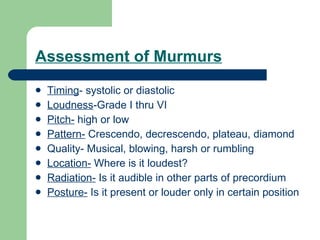
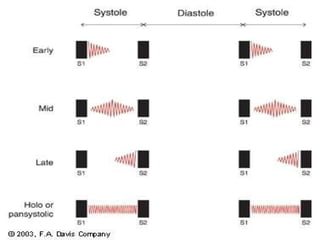
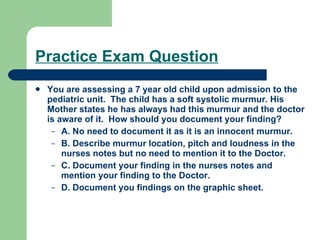
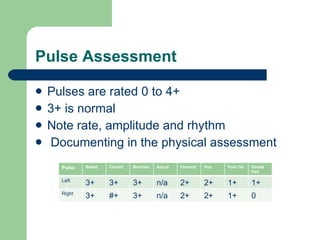
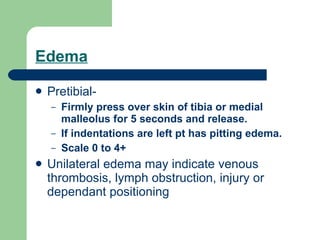
This document provides information on assessing the cardiovascular and peripheral vascular systems. It describes how to inspect, palpate, percuss and auscultate various structures including neck vessels, jugular veins, precordium, apical pulse, heart sounds, murmurs, and peripheral pulses and limbs. Specific assessment techniques are provided for different age groups.