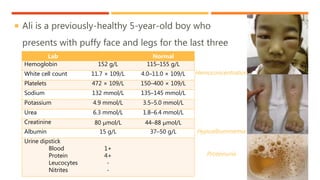
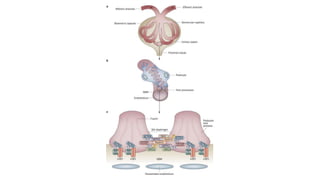
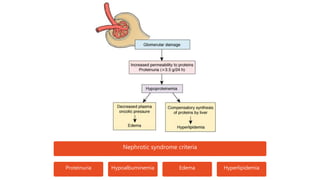
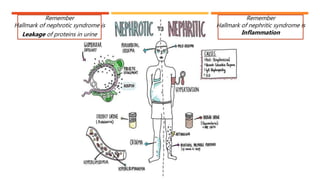
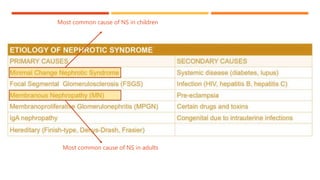
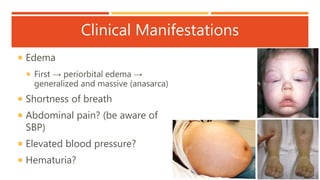
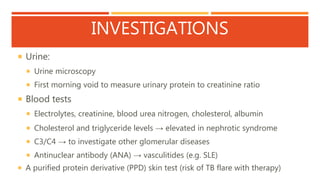
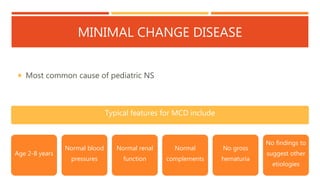
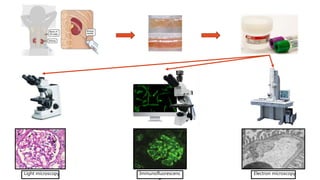
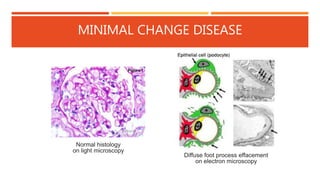
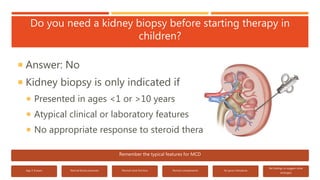
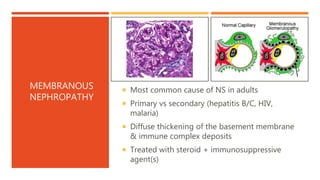
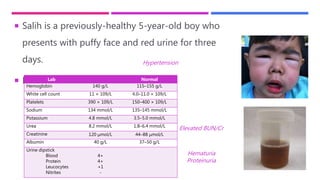
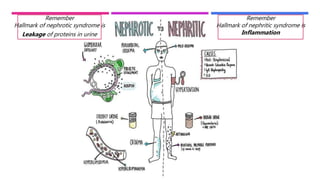
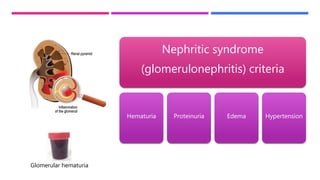
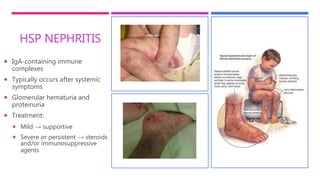
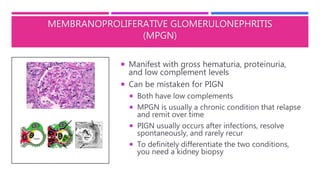
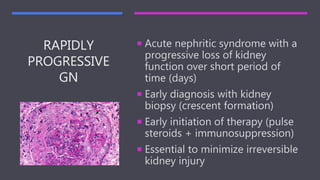
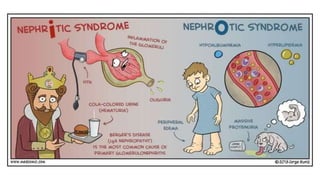
This document discusses nephrotic and nephritic syndrome. It begins by presenting the case of a 5-year-old boy, Ali, who presents with puffy face and legs. His lab work shows hypoalbuminemia and proteinuria consistent with nephrotic syndrome criteria. The document then defines nephrotic and nephritic syndrome, discusses their causes and clinical manifestations. It covers investigations, complications, treatment including for minimal change disease, membranous nephropathy and focal segmental glomerulosclerosis. The document also presents another case of nephritic syndrome and discusses causes of glomerulonephritis in children such as IgA nephropathy, membranoprolifer