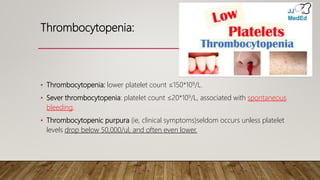
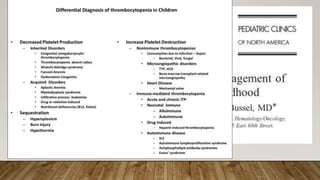
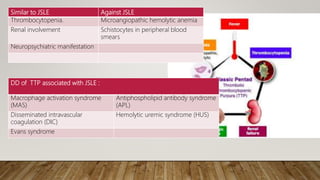
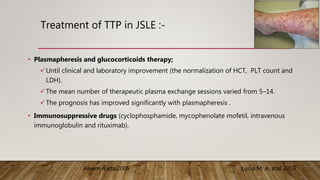
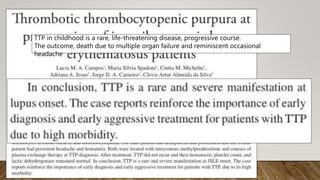
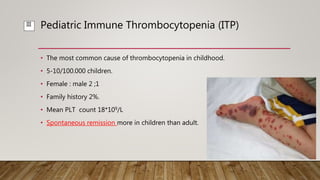
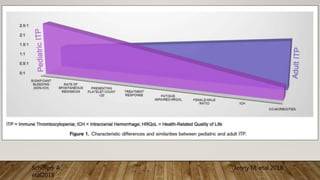
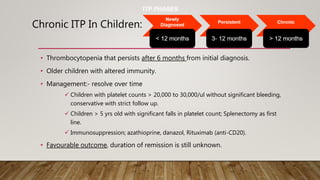
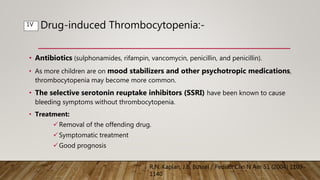
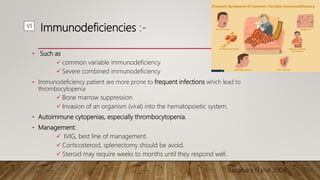
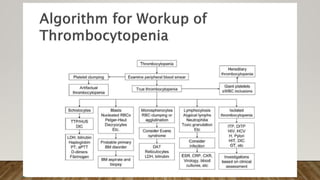
This document discusses various causes of thrombocytopenia in pediatrics, including immune thrombocytopenia (ITP), which is the most common cause in children. Drug-induced thrombocytopenia and thrombocytopenia associated with conditions like lupus and thrombotic thrombocytopenic purpura (TTP) are also reviewed. Management strategies for different types of thrombocytopenia are provided, such as observation for mild ITP, IVIG and steroids as first-line ITP treatment, and plasmapheresis and immunosuppression for TTP. Rare causes like Fanconi anemia and bone marrow involvement from cancers are also summarized.