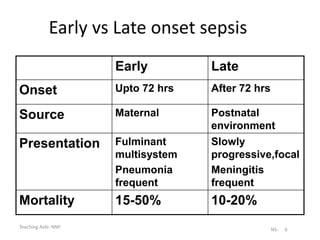
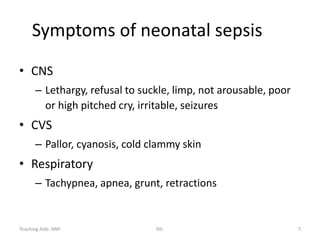
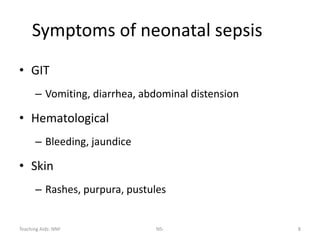
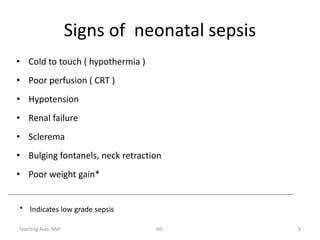
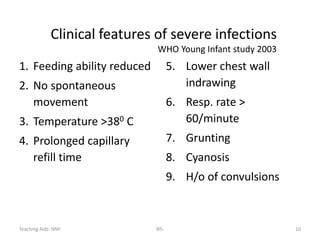
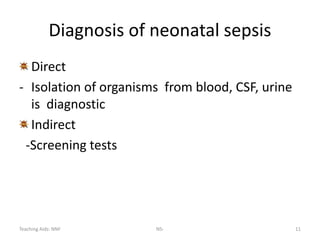
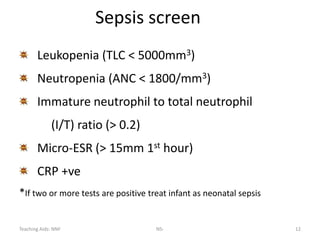
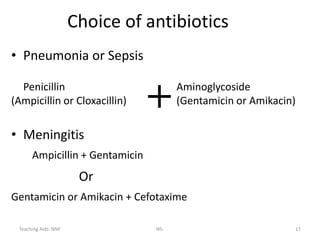
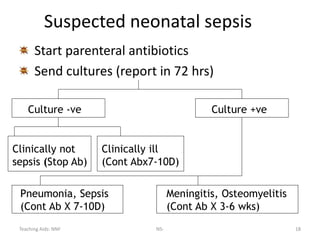
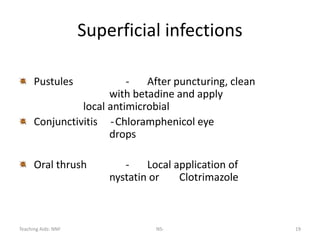
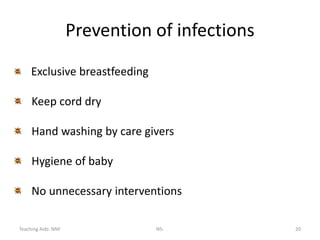
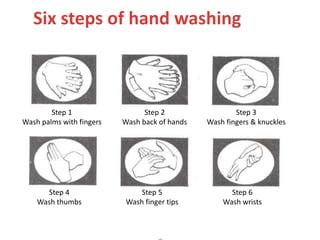
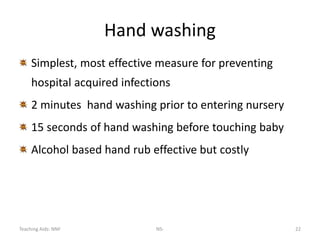
Neonatal sepsis is a major cause of neonatal mortality in developing countries, contributing to about 30-50% of deaths. The incidence of neonatal sepsis in India is approximately 30 per 1000 live births. Sepsis can be either early-onset (within 72 hours of birth) or late-onset, and is usually caused by organisms like Klebsiella pneumoniae, E. coli, and Staphylococcus aureus. Diagnosis involves clinical signs and symptoms as well as screening tests and blood/CSF cultures. Treatment consists of supportive care and parenteral antibiotics like ampicillin and aminoglycosides. Prevention emphasizes handwashing, hygiene, and infection control practices.