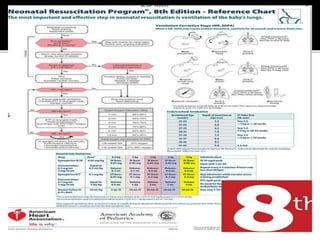
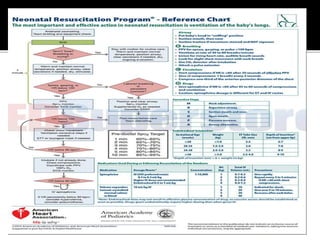
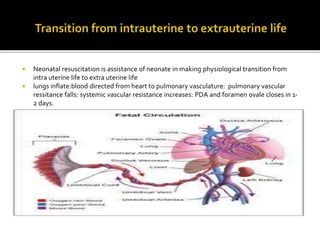
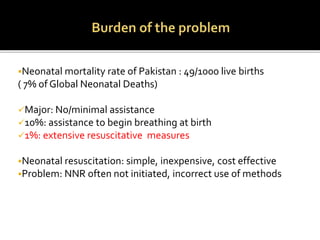
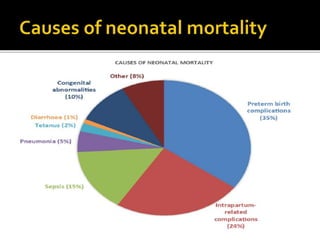
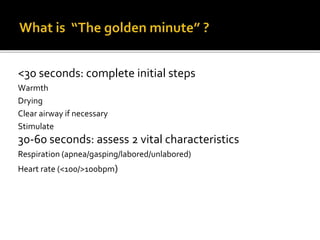
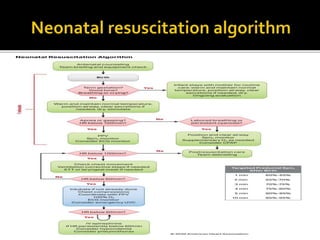
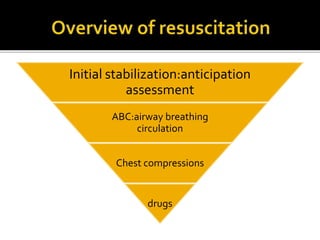
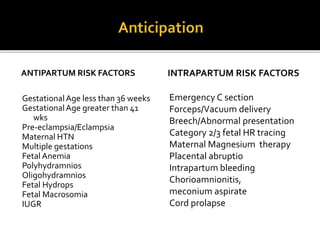
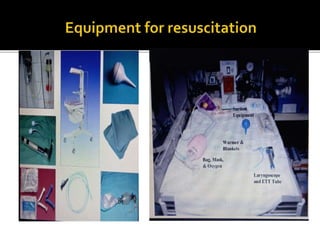
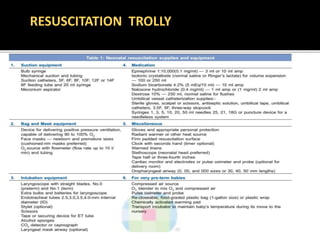
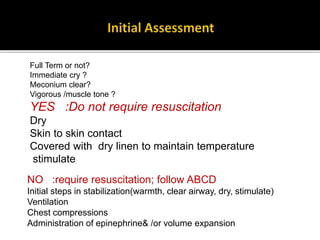
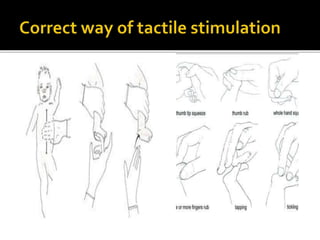
Neonatal resuscitation is critical to assist newborns in transitioning from intrauterine to extrauterine life. The steps include warming, drying, clearing the airway if needed, and stimulating the baby. Assessment of heart rate and respiration are important to determine if further resuscitation is required, such as ventilation, chest compressions, epinephrine or volume expansion. Proper resuscitation requires anticipating at-risk babies, assessing the newborn, and providing ABC support which may include medical intervention. Thorough documentation and monitoring in the NICU is important for newborn outcome.






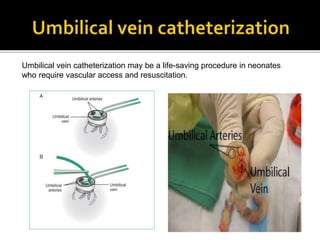
![ After proper placement of the umbilical line, intravenous
(IV) fluids and medication may be administered to critically ill
neonates.[1]
In an emergency, it is best to advance the catheter only 1-2
cm beyond the point at which good blood return is obtained
so as to avoid injecting hyperosmolar fluids into the portal
vessels and causing liver necrosis.](https://image.slidesharecdn.com/neonatalresuscitation-230809112158-80cda122/85/NEONATAL-RESUSCITATION-pptx-51-320.jpg)