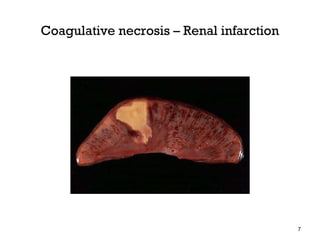
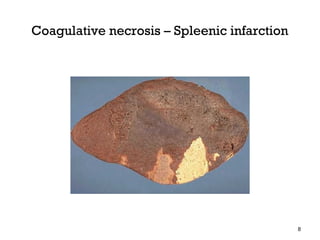
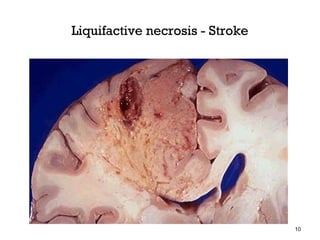
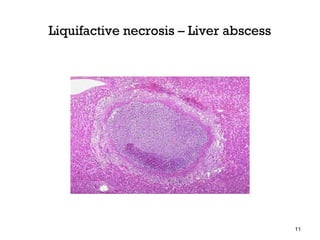
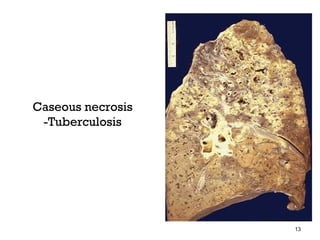
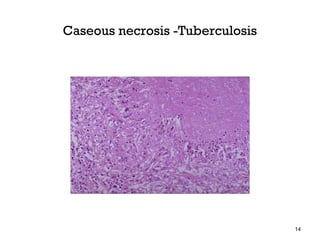
This document defines and describes different types of necrosis. It begins by defining necrosis as focal death and degradation of tissue by hydrolitic enzymes, accompanied by inflammation. It then describes several types of necrosis including coagulative, liquefactive, caseous, fat, and fibrinoid necrosis. Coagulative necrosis is the most common type caused by ischemia. Liquefactive necrosis occurs due to enzymatic degradation. Caseous necrosis is seen in tuberculosis. Fat necrosis occurs in the pancreas and breast. Fibrinoid necrosis involves fibrin deposition. The document also discusses pathologic changes seen in different types of necrosis both grossly and microscopically.