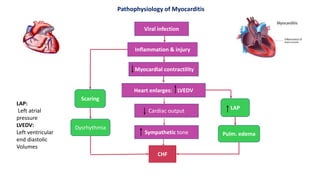
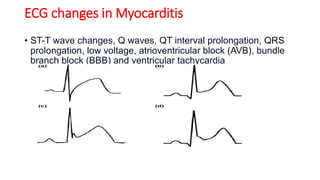
Myocarditis is an inflammatory disease of the myocardium caused by various infectious and non-infectious triggers, leading to symptoms such as chest pain and shortness of breath. It can result in significant complications like heart failure and arrhythmias, with diagnoses relying on ECG changes and lab tests. Treatment involves managing cardiac decompensation through medications, immunosuppressive therapy, and supportive care, while nursing management focuses on monitoring and reducing cardiac workload.