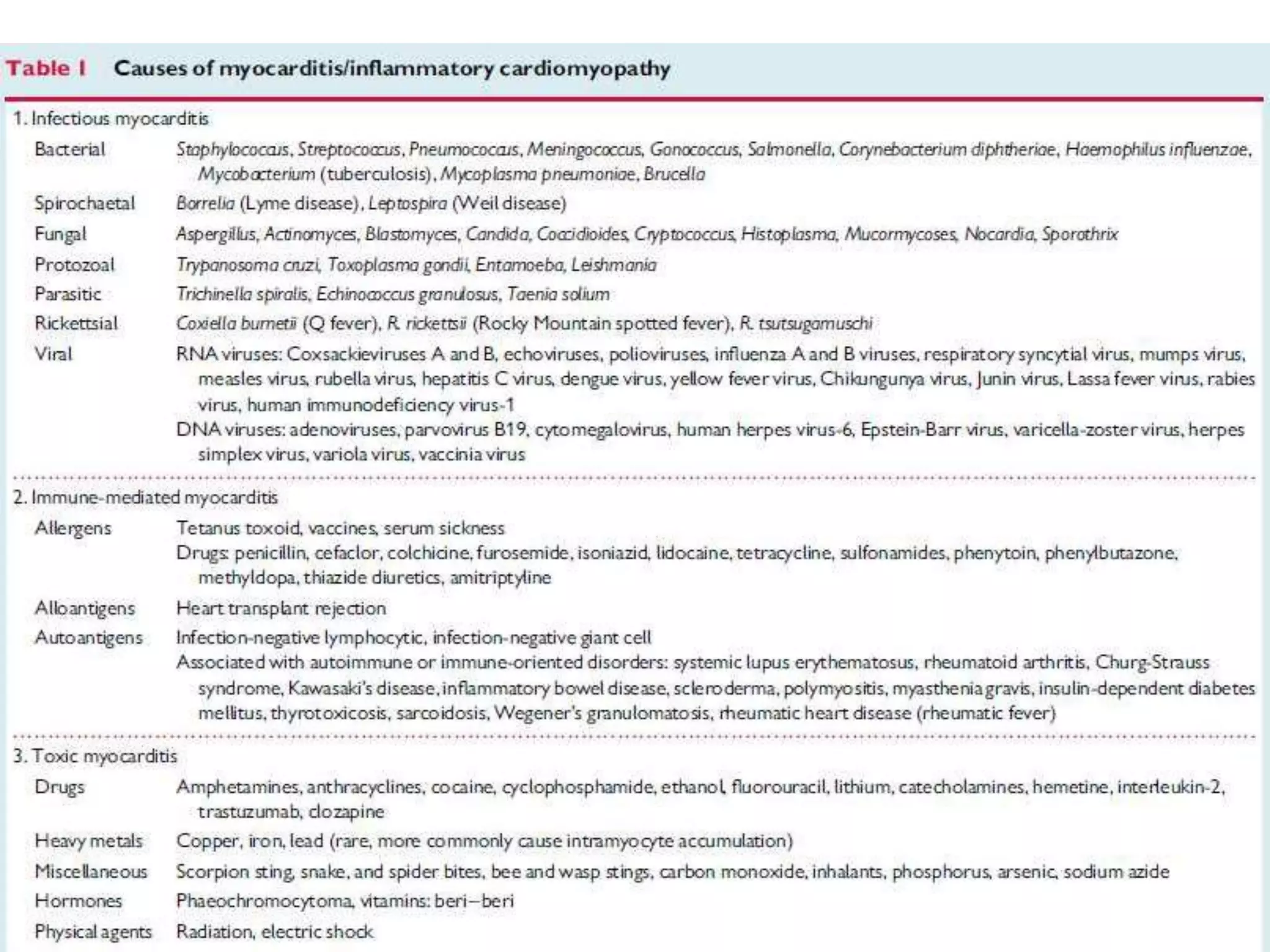
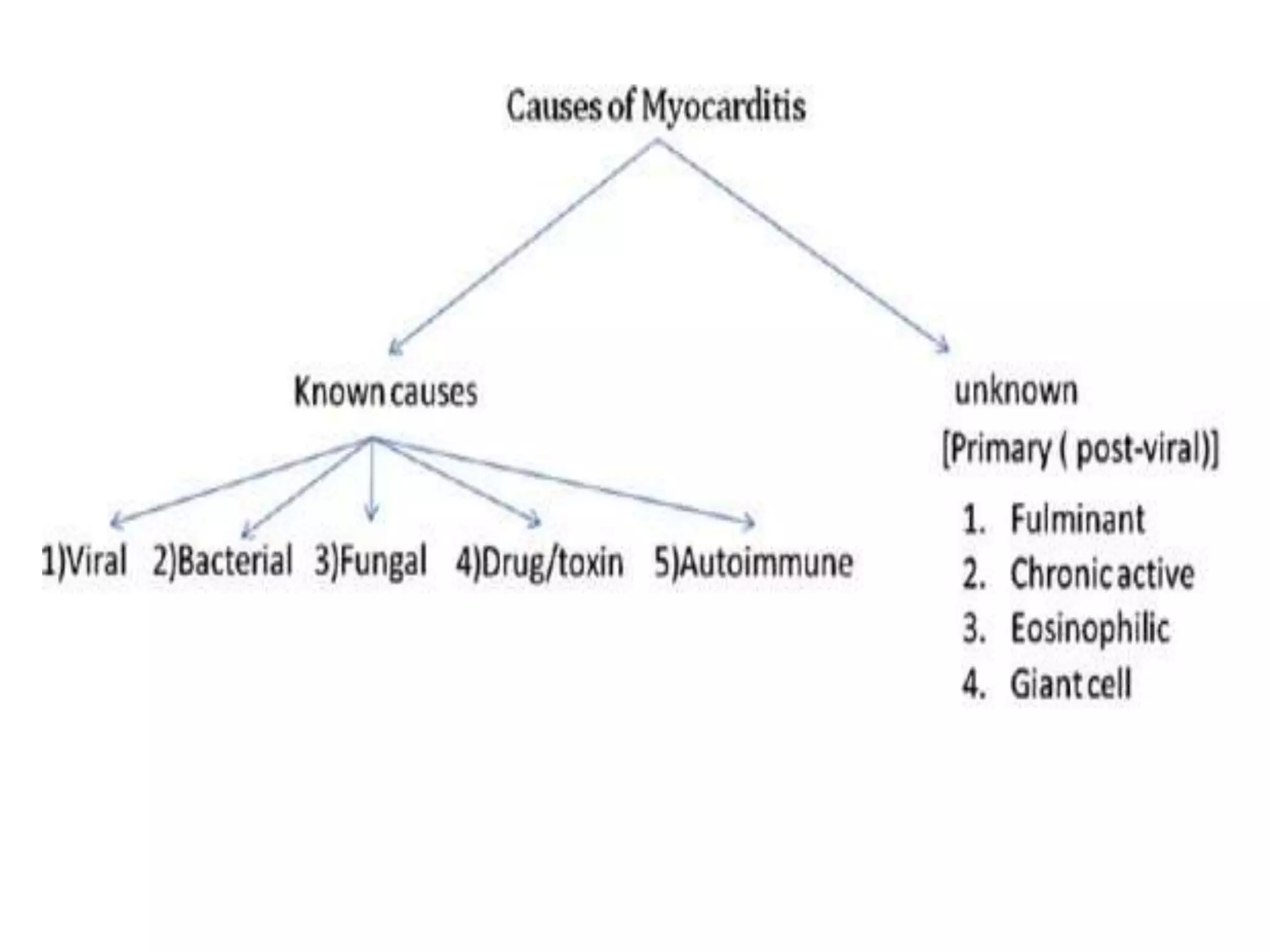
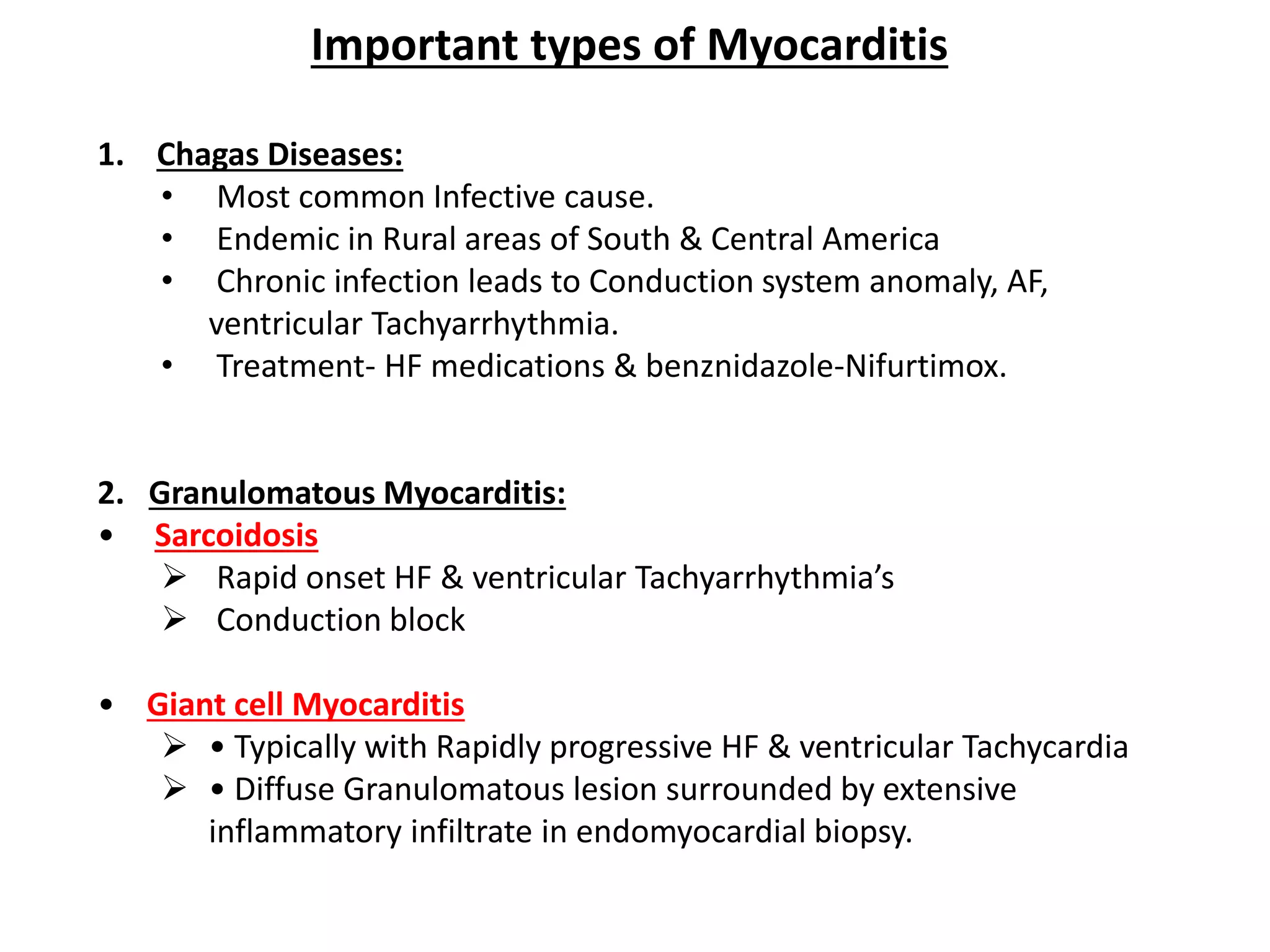
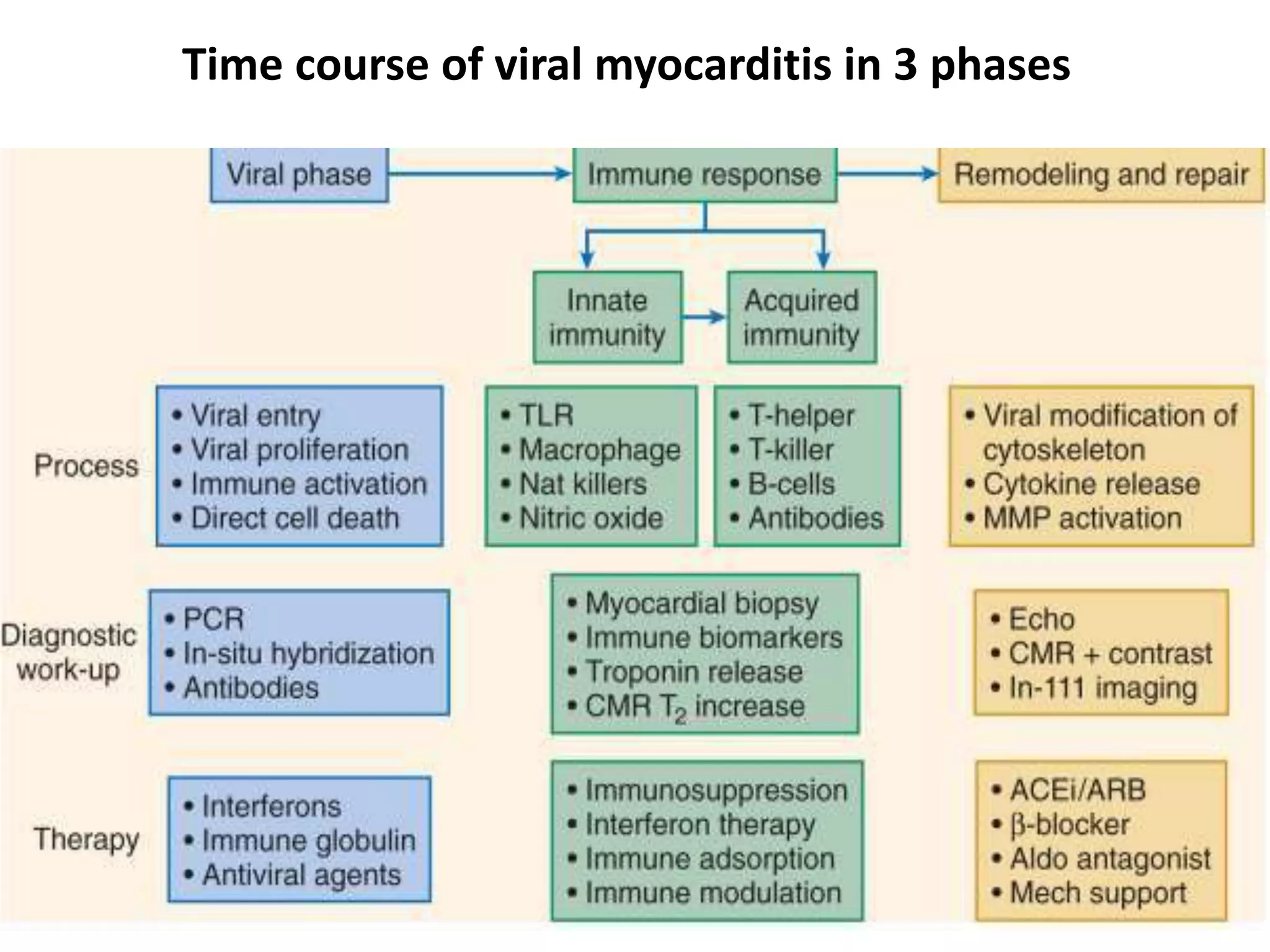
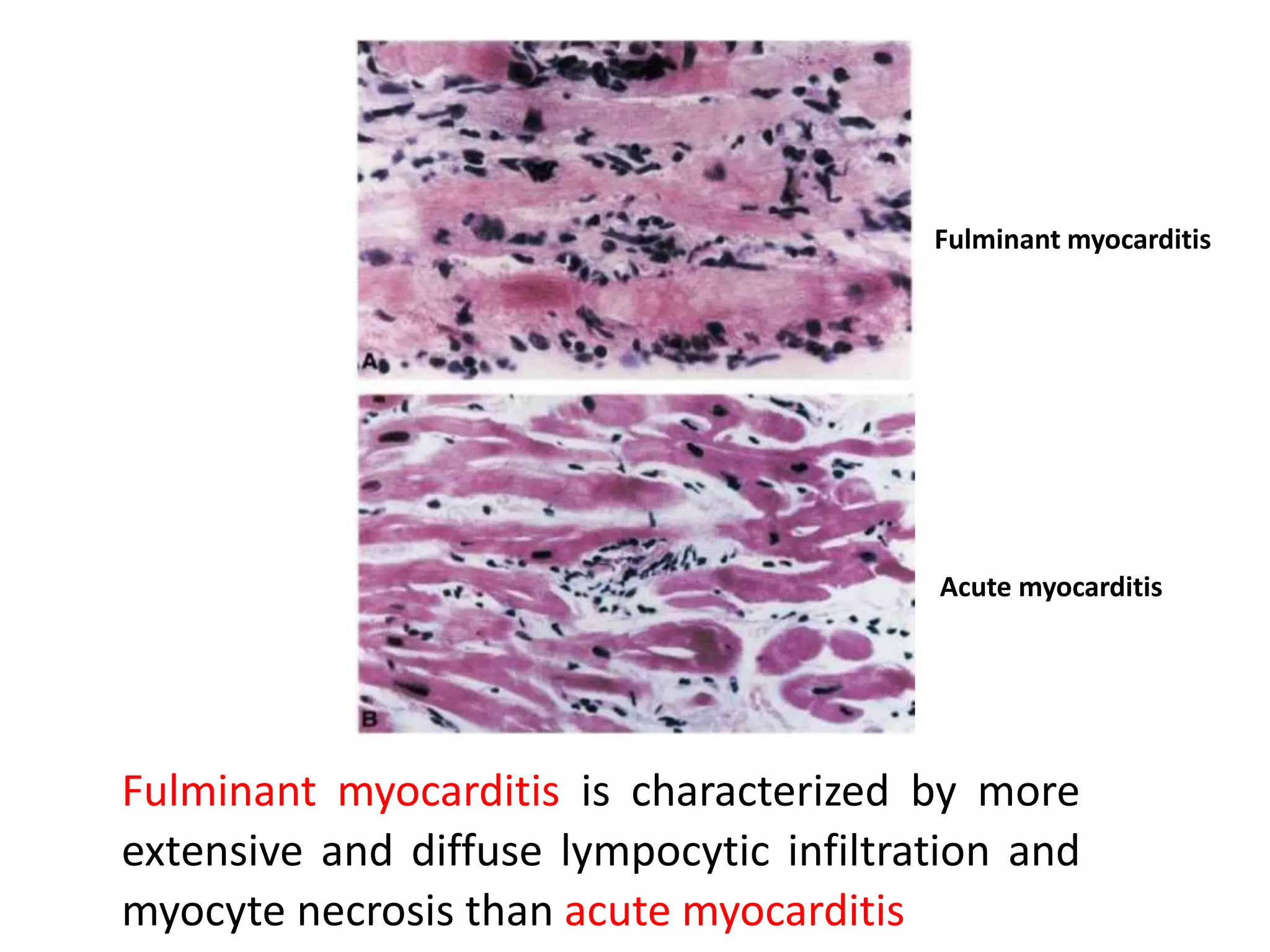
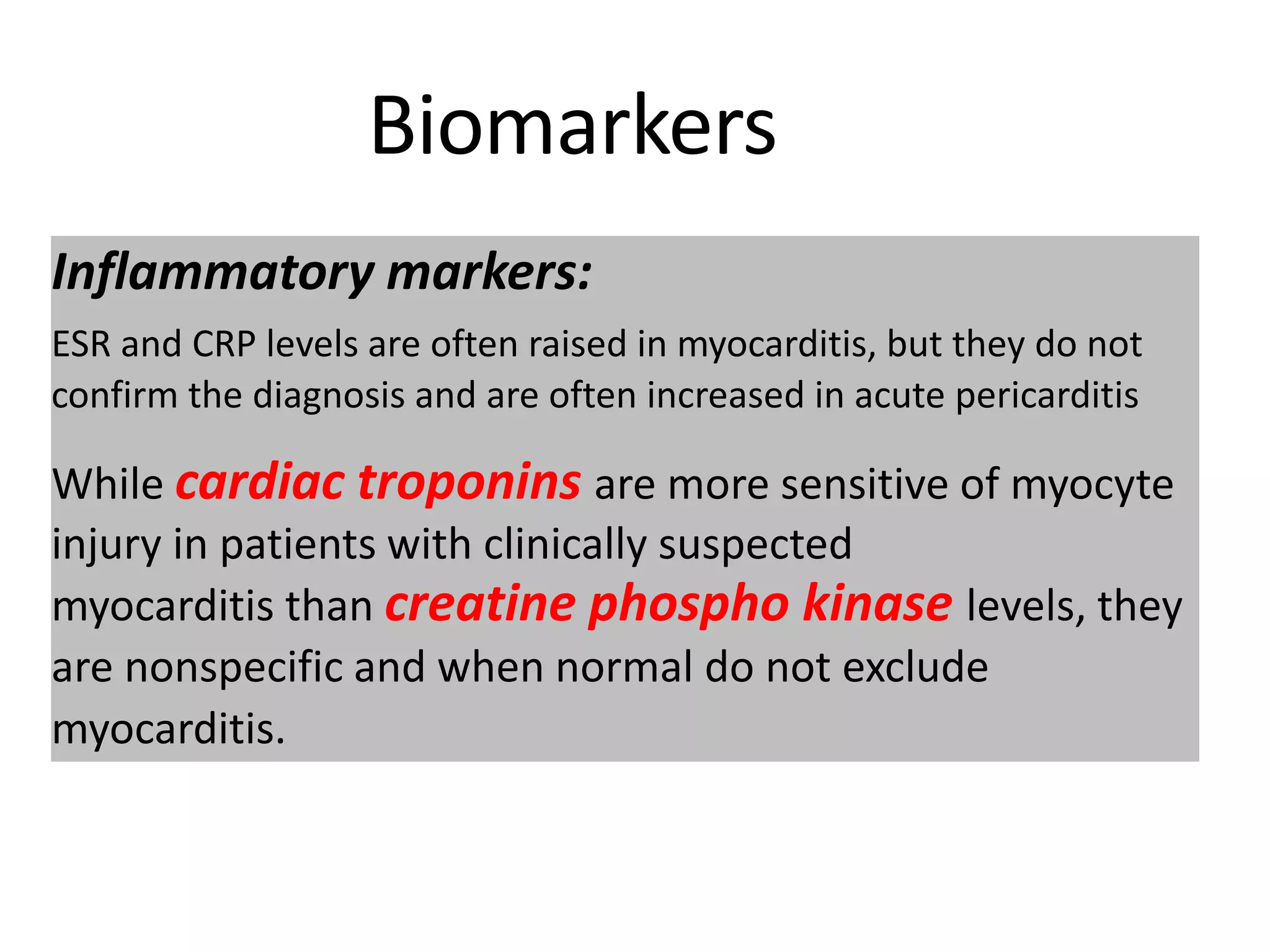
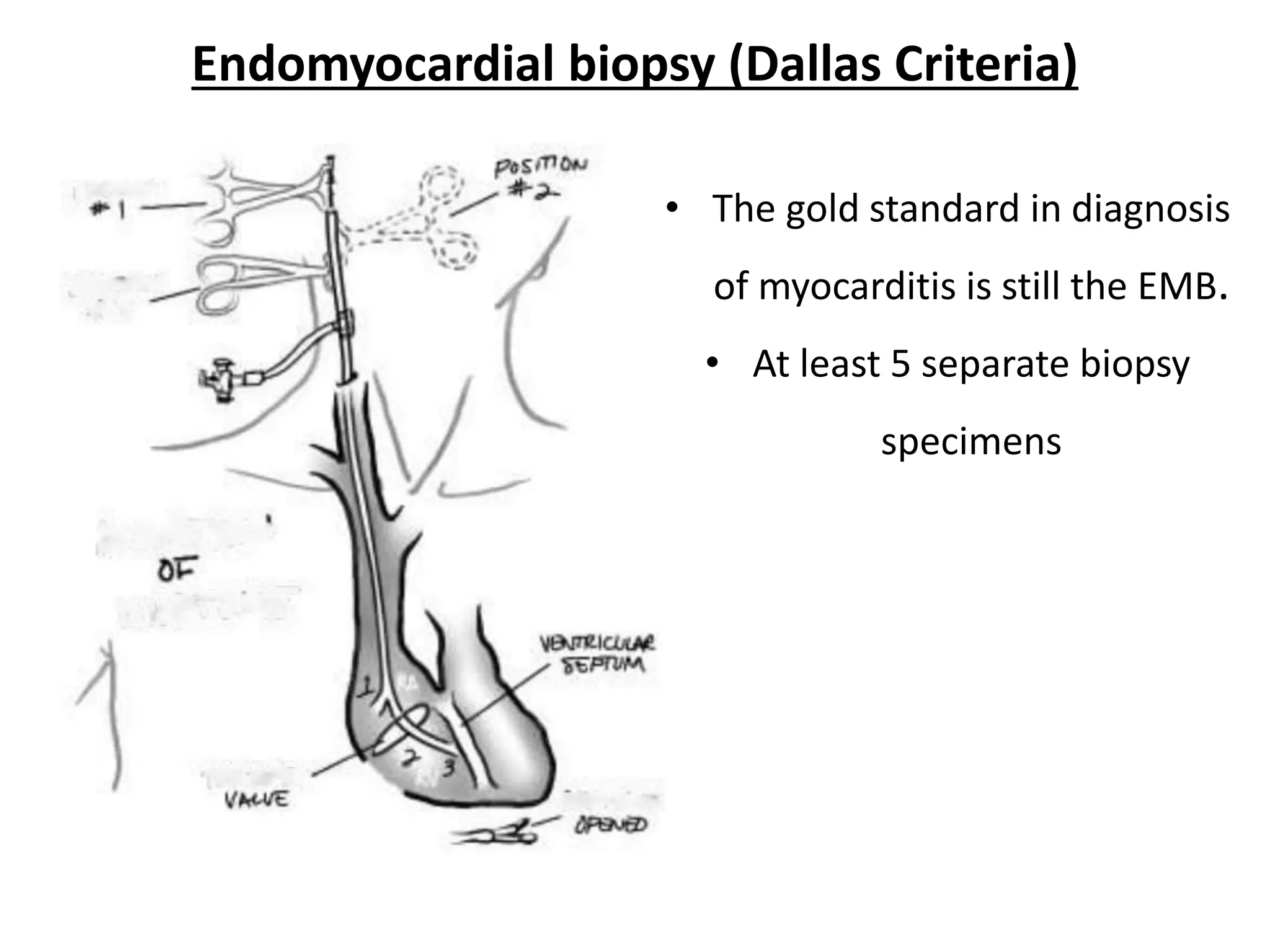
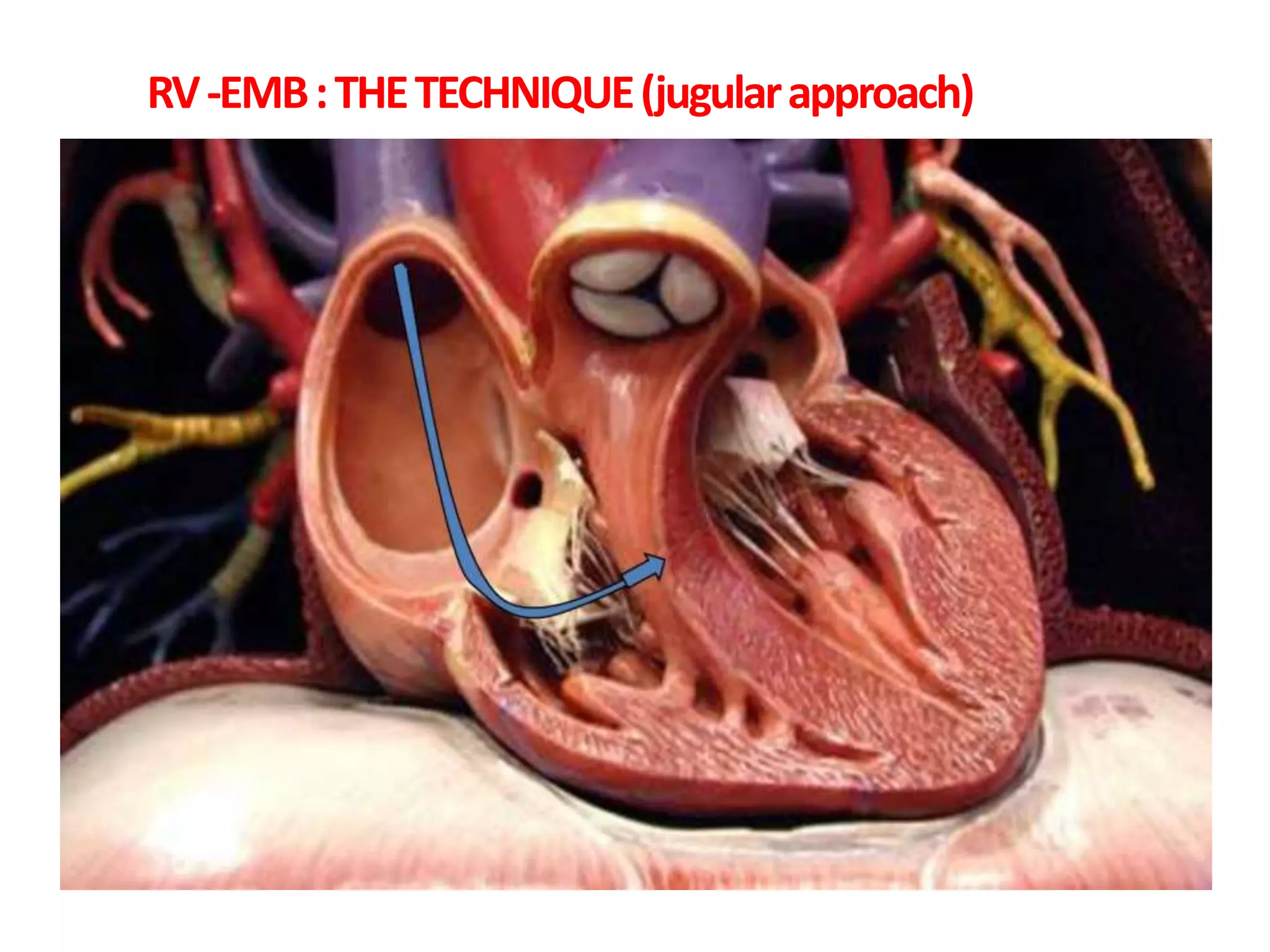
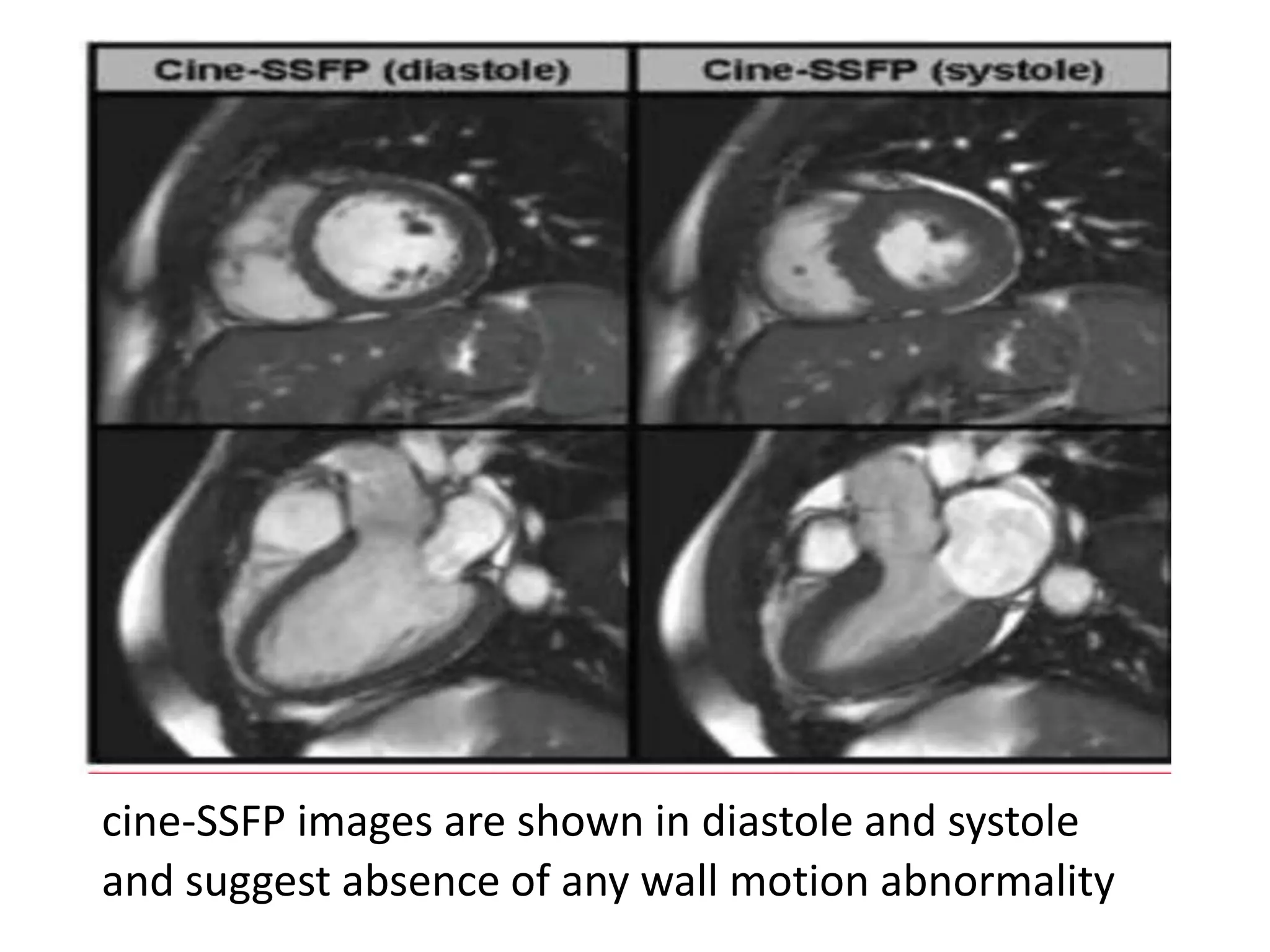
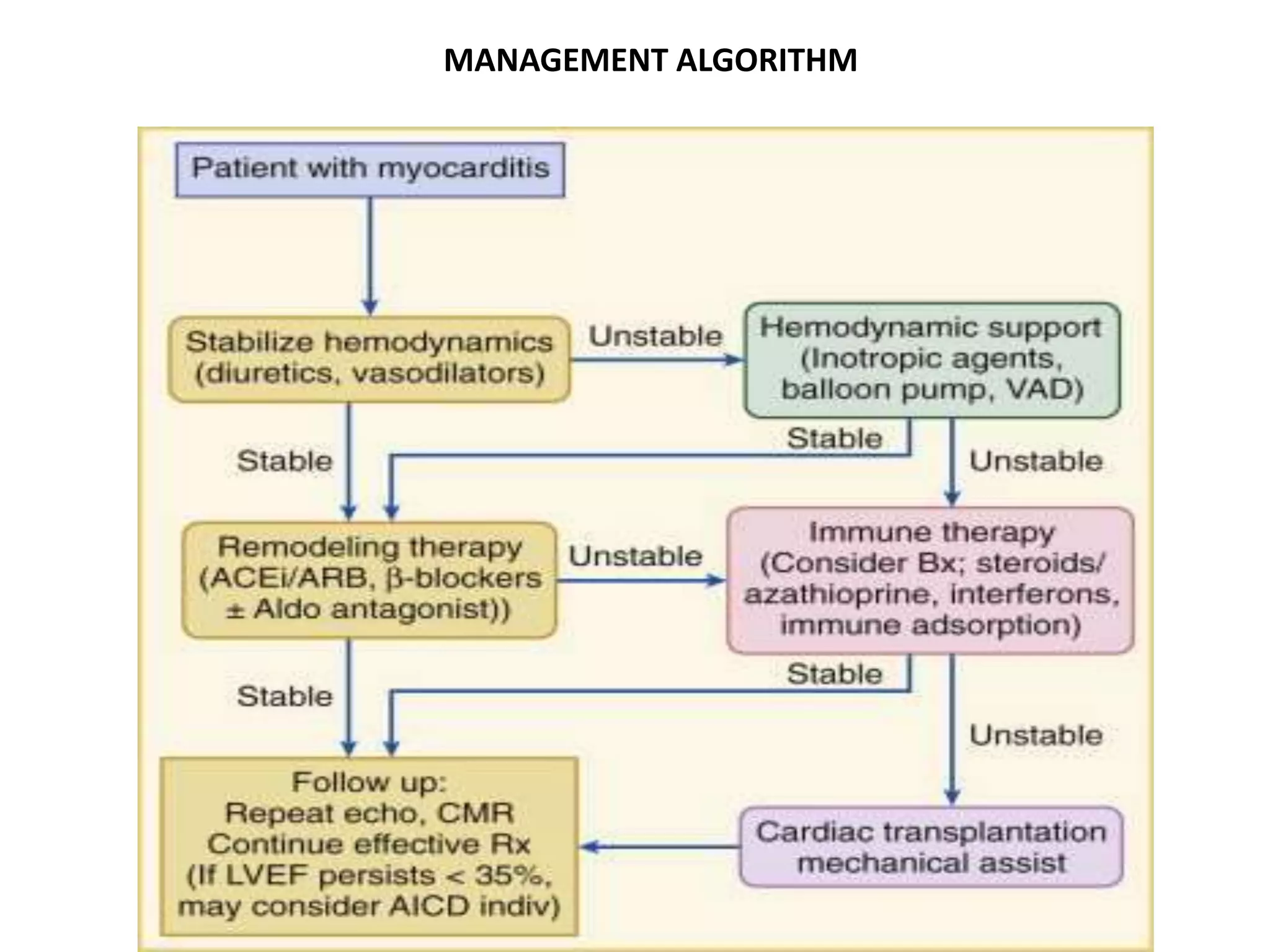
Myocarditis is an inflammatory disease of the heart muscle (myocardium) that can be caused by infections or non-infectious triggers. It has variable presentations ranging from mild chest pain to life-threatening cardiogenic shock. Diagnosis involves ECG, cardiac enzymes, echocardiogram, cardiac MRI and endomyocardial biopsy. Treatment focuses on managing arrhythmias, heart failure, and restricting activity in the acute phase. While many cases resolve, some can lead to persistent heart dysfunction or dilated cardiomyopathy.