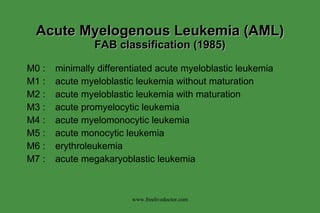
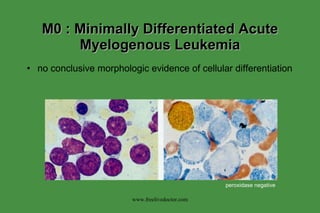
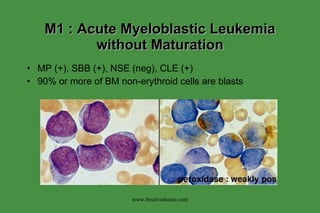
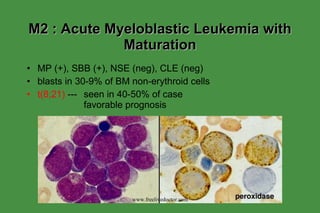
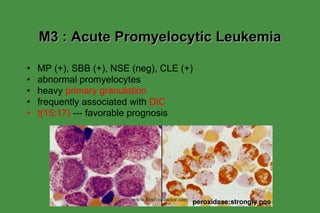
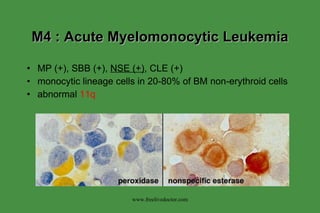
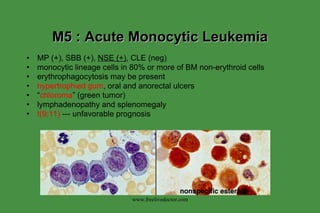
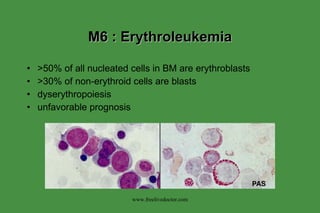
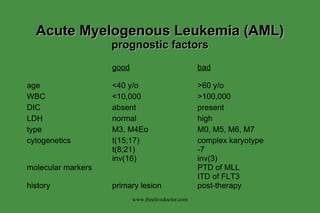
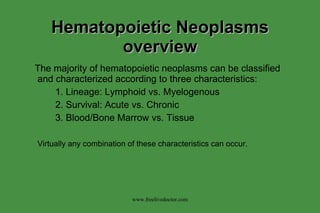
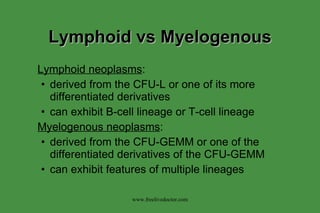
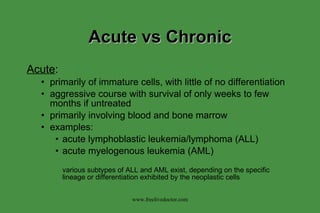
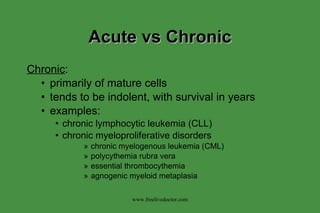
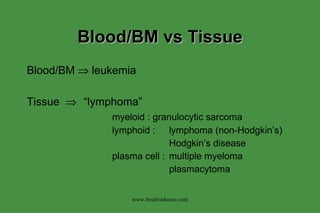
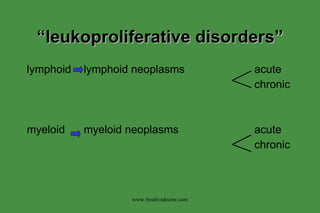
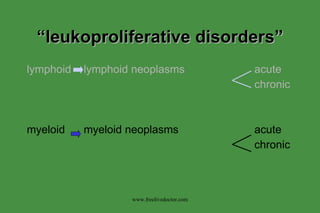
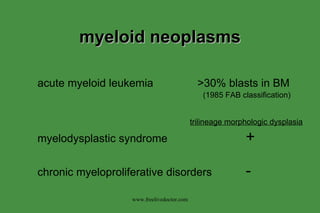
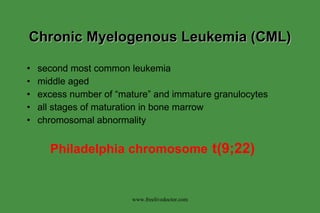
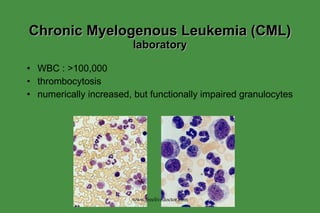
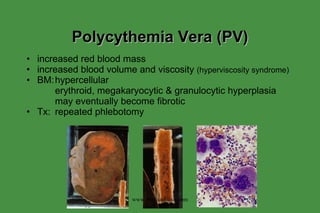
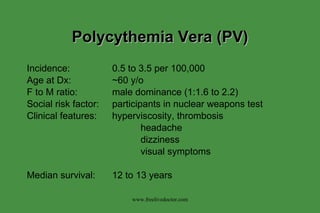
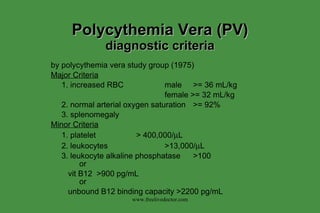
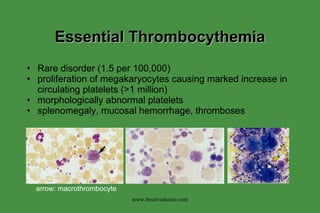
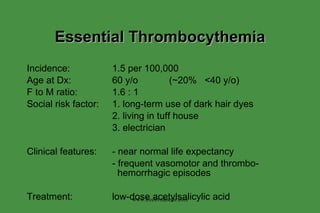
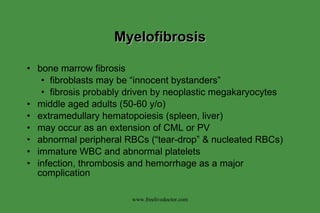
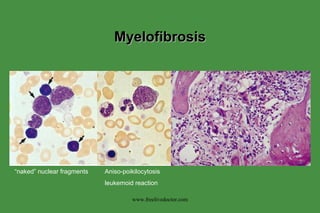
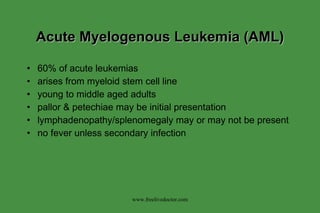
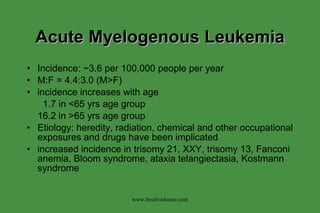
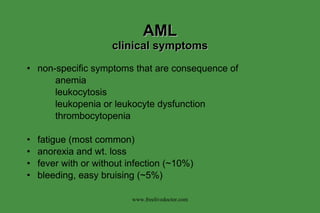
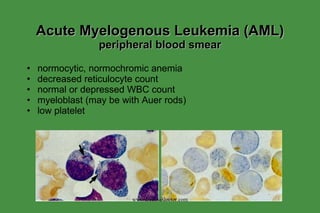
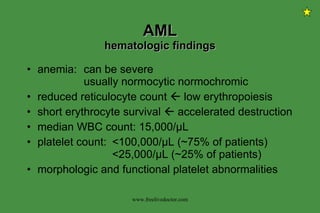
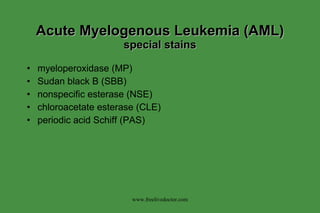
The document discusses hematopoietic neoplasms and myeloproliferative disorders. It describes how hematopoietic neoplasms can be classified based on lineage, chronicity, and location. It then focuses on chronic myeloproliferative disorders including chronic myelogenous leukemia, polycythemia vera, essential thrombocythemia, myelofibrosis, and their characteristics and diagnostic criteria. Acute myelogenous leukemia is also discussed.

![Chronic Myeloproliferative Disorders (new WHO classification) 1. polycythemia vera 2. chronic idiopathic myelofibrosis 3. essential thrombocytosis 4. chronic myeloid leukemia (CML) 5. [chronic neutrophilic leukemia] 6. [chronic eosinophilic leukemia] 7. [hypereosinophilic syndrome] “ myelodysplastic/myeloproliferative diseases” juvenile myelomonocytic leukemia atypical chronic myeloid leukemia (lacking t(9;22)) chronic myelomocytic leukemia www.freelivedoctor.com](https://image.slidesharecdn.com/myeloproliferative-100416234024-phpapp02/85/Myeloproliferative-12-320.jpg)

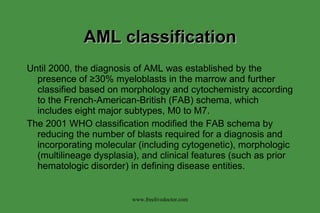
![Acute Myelogenous Leukemia (AML) WHO classification (2001) I. AML with rucurrent genetic abnormalities AML with t(8;21)(q22;q22);AML1(CBF α )/ETO AML with abnormal bone marrow eosinophils [inv(16)(p13q22) or t(16;16)(p13;q22);CBF β /MYH11] Acute promyelocytic leukemia [AML with t(15;17)(q22;q12) (PML/RAR α and variants] AML with 11q23 (MLL) abnormalities II. AML with multilineage dysplasia Following a myelodysplastic syndrome or myelodysplastic syndrome/myeloproliferative disorder Without antecedent myelodysplastic syndrome III. AML and myelodysplastic syndromes, therapy-related Alkylating agent-related Topoisomerase type II inhibitor-related Other types IV. AML not otherwise categorized AML minimally differentiated AML without maturation AML with maturation Acute myelomonocytic leukemia Acute monoblastic and monocytic leukemia Acute erythroid leukemia Acute megakaryoblastic leukemia Acute basophilic leukemia Acute panmyelosis with myelofibrosis Myeloid sarcoma ≥ 20% myeloblasts in blood and/or bone marrow = AML positive myeloperoxidase reaction in >3% of blasts = AML (↔ ALL) www.freelivedoctor.com](https://image.slidesharecdn.com/myeloproliferative-100416234024-phpapp02/85/Myeloproliferative-32-320.jpg)