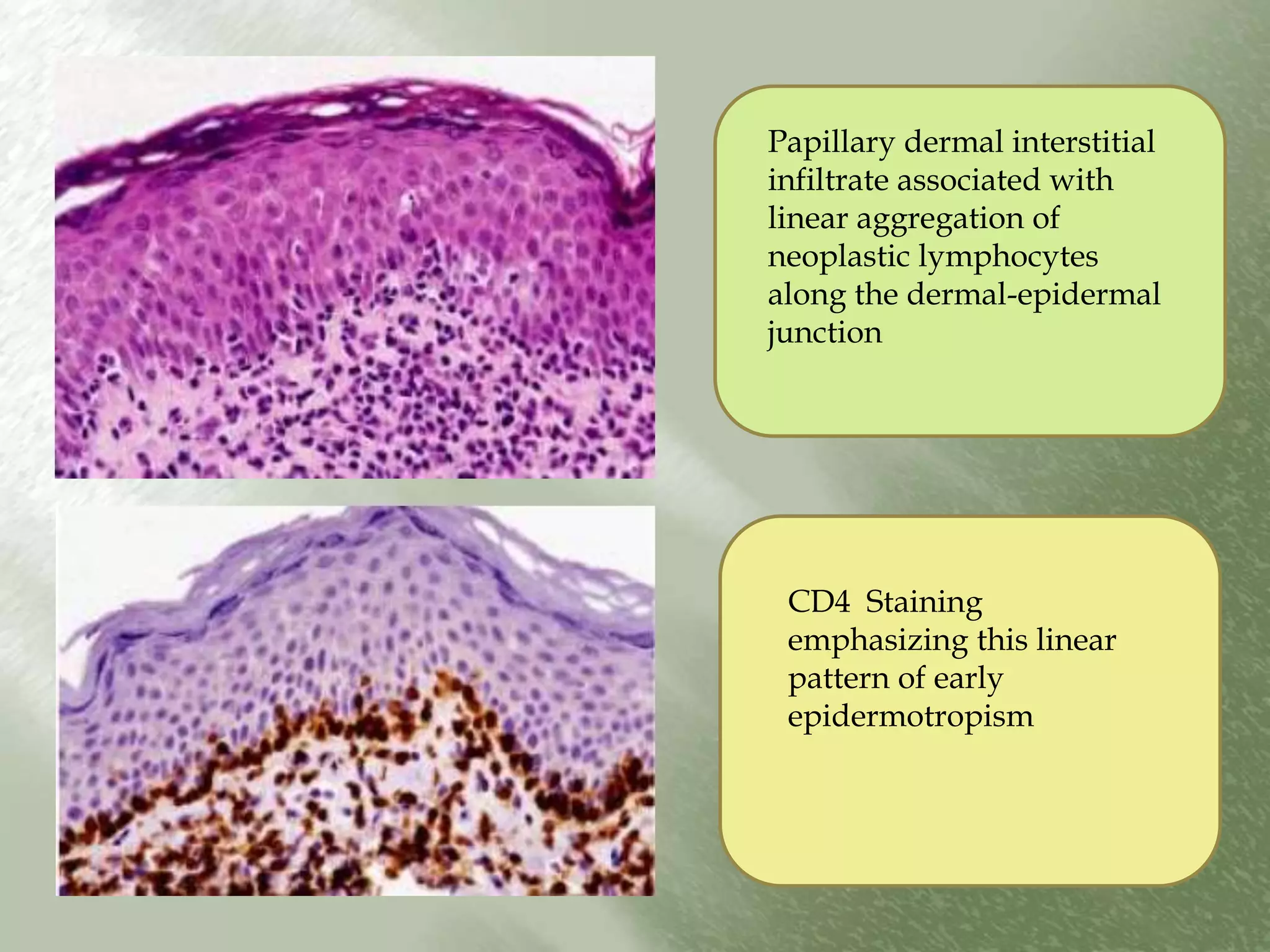
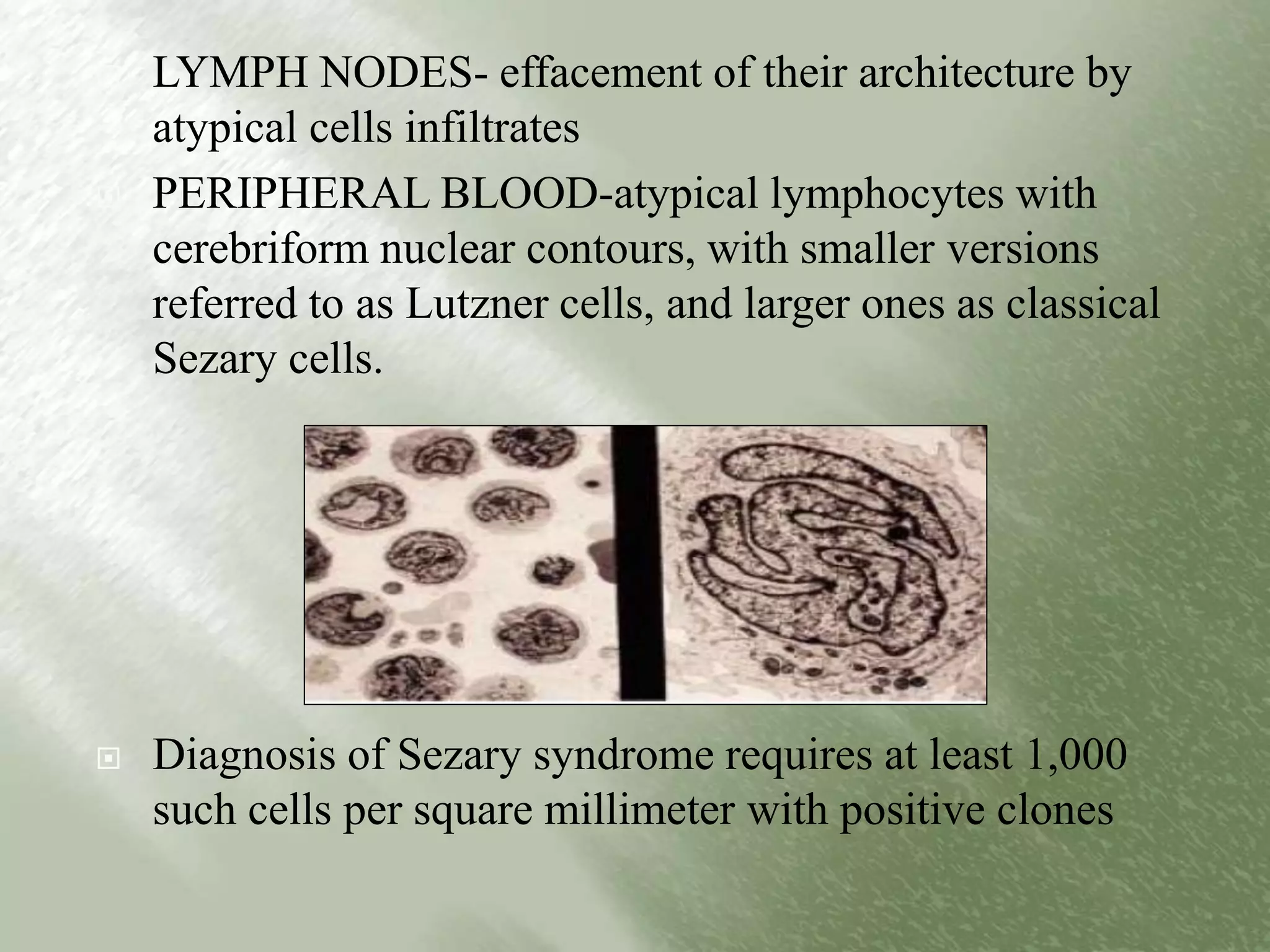
The document discusses various types of cutaneous lymphomas, focusing on primary and secondary forms, and the distinct behaviors and characteristics of T-cell and B-cell lymphomas. It elaborates on diagnostic criteria, clinical features, and histopathologic presentations for conditions like mycosis fungoides and Sezary syndrome. Additionally, it outlines the immunological responses and migration patterns of lymphocytes within the skin, highlighting the complex nature of these diseases.