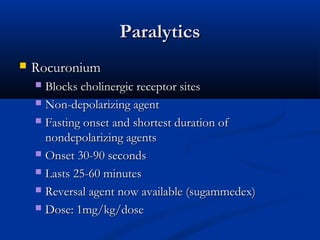
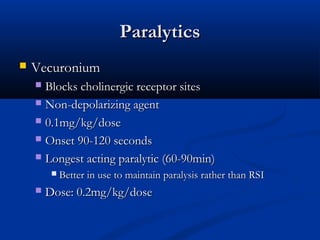
This document discusses medications used for pediatric resuscitation and rapid sequence intubation (RSI). It reviews sedatives like etomidate, midazolam, thiopental and ketamine, analgesics like fentanyl, paralytics like succinylcholine, rocuronium and vecuronium, and pre-medications like atropine and lidocaine. For each drug, it provides information on pharmacology, dosing, indications, side effects and special considerations in pediatrics. The goal is to discuss best practices for medication selection and administration during pediatric resuscitations and RSI.