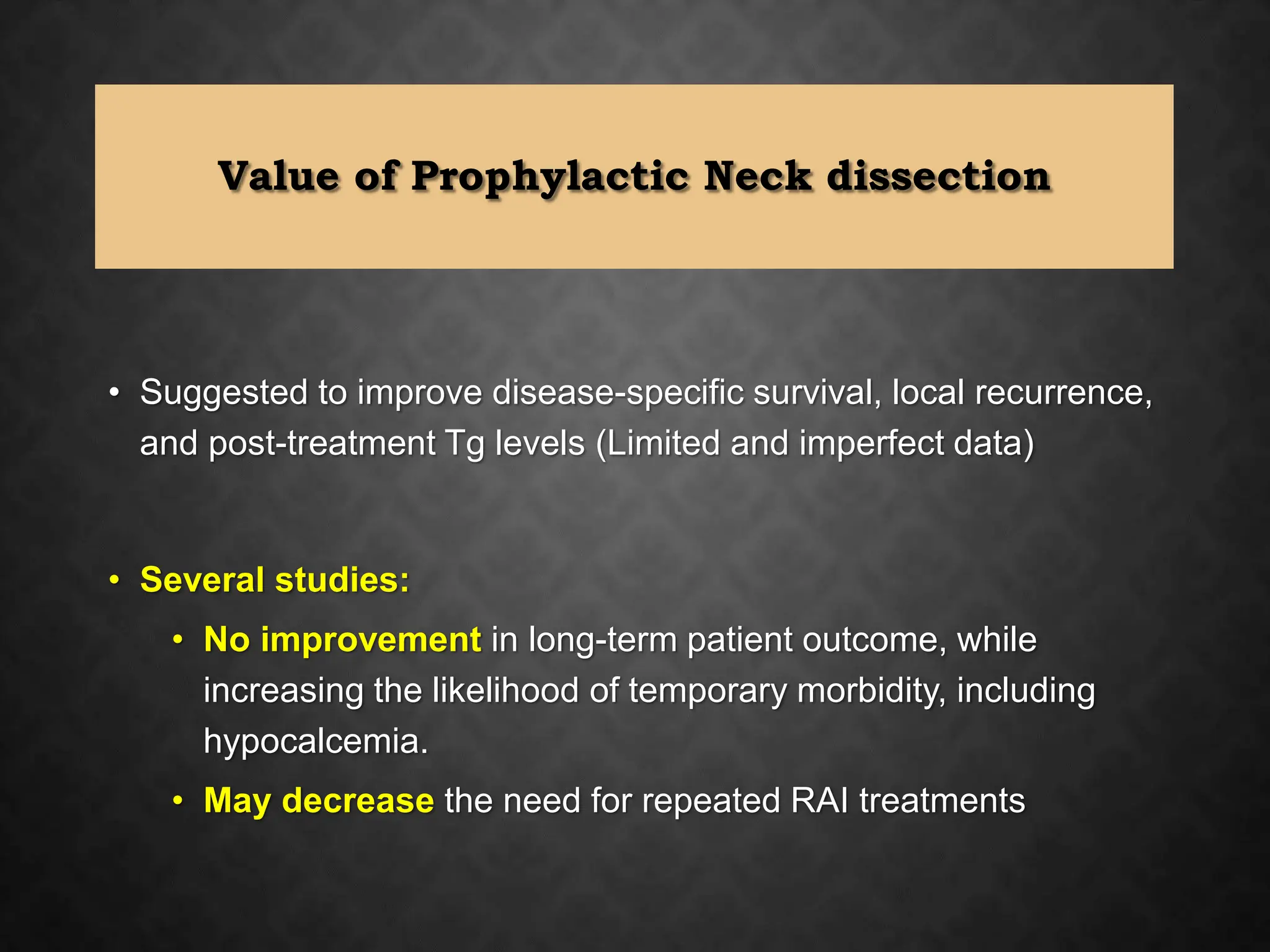
The 2015 American Thyroid Association guidelines outline the management strategies for thyroid nodules and differentiated thyroid cancer, emphasizing the importance of histological diagnosis and appropriate surgical interventions. Lobectomy is recommended for solitary indeterminate nodules, while total thyroidectomy may be indicated based on certain risk factors. The guidelines also detail the goals of initial therapy for differentiated thyroid carcinoma, which include improving survival rates and accurate disease staging, alongside discussions about the role of postoperative care and risk stratification.



![• Primary goal: To establish a histological diagnosis and definitive
removal, while reducing the risks associated with remedial
surgery in the previously operated field if the nodule proves to be
malignant
• Appropriate surgeries:
• Lobectomy (hemithyroidectomy) with or without
isthmusectomy,
• Near-total thyroidectomy: Removal of all grossly visible
thyroid tissue, leaving only a small amount [<1 g] of tissue
adjacent to the recurrent laryngeal nerve near the ligament of
Berry, or
• Total thyroidectomy : Removal of all grossly visible thyroid](https://image.slidesharecdn.com/ataguidelinesmanagement-240626140223-f069730a/75/ATA-GUIDELINES-MANAGEMENT-for-otolaryngology-pptx-5-2048.jpg)