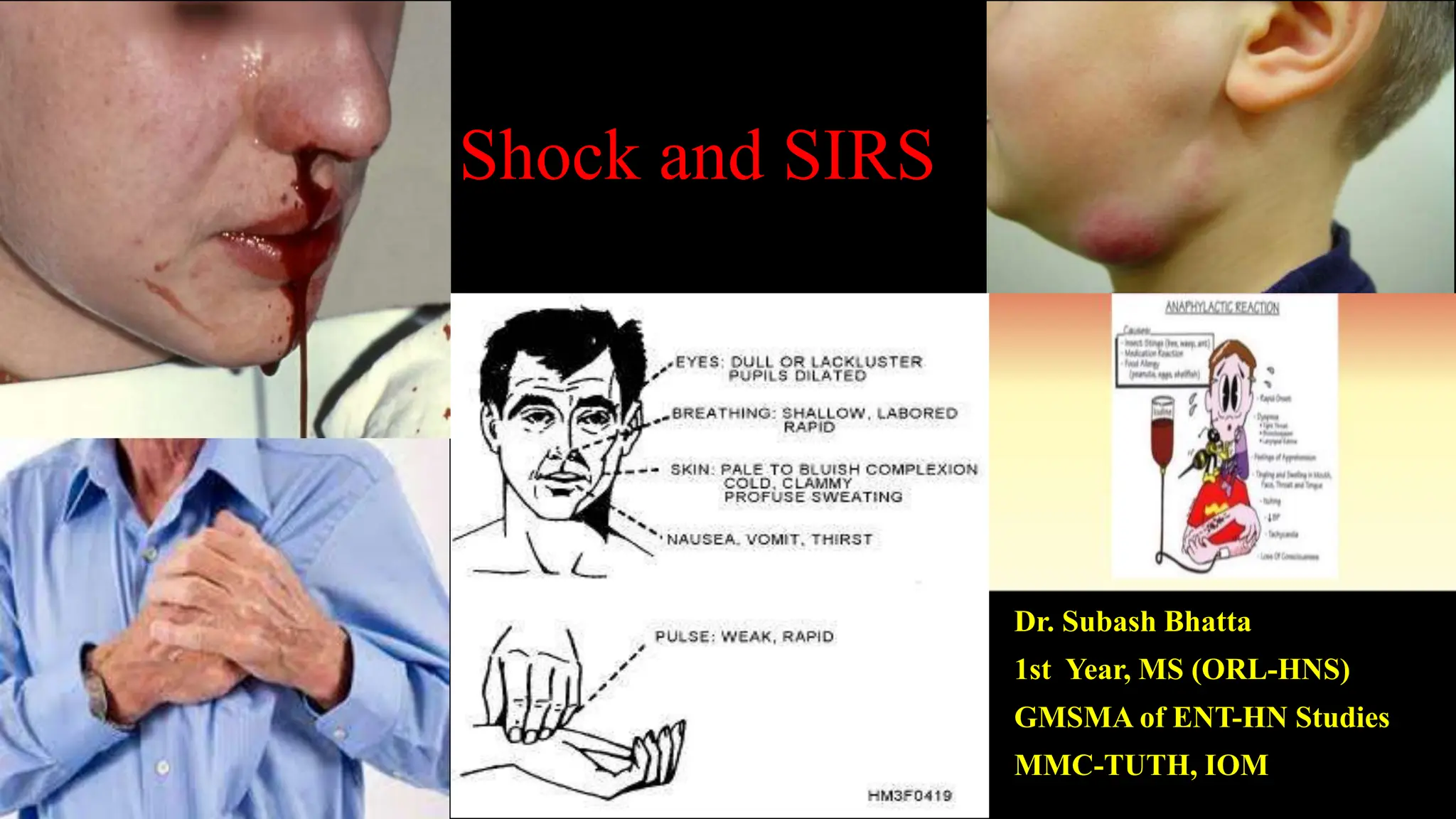
The document provides a comprehensive overview of shock and systemic inflammatory response syndrome (SIRS), detailing various types including hypovolemic, cardiogenic, obstructive, and distributive shock. It includes definitions, historical perspectives, pathophysiology, clinical manifestations, and management strategies for each type, highlighting the significance of adequate perfusion and timely intervention to prevent organ failure and death. Special focus is given to the most common causes of shock in Nepal, such as road traffic accidents and the recent earthquake.



































![Cardiogenic shock
Life-threatening medical condition resulting from an
inadequate circulation of blood due to primary failure of
the ventricles of the heart to function effectively
Characterized by systemic hypo perfusion due to severe
depression of the cardiac index [<2.2 (L/min)/m2] and
sustained systolic arterial hypotension (<90 mmHg) despite
an elevated filling pressure [pulmonary capillary wedge
pressure (PCWP) >18 mmHg].
Ciculatory shock
Insufficient perfusion of tissue to meet the demands for oxygen and nutrients](https://image.slidesharecdn.com/jhhrn8gq8qmjqmi9sytt-shock-and-sirs-240509182821-ab9c1a90/75/shock_and_sirs-in-basic-otolaryngology-pptx-37-2048.jpg)





























































