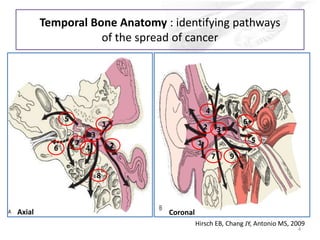
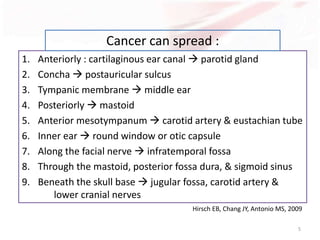
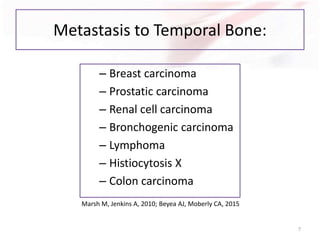
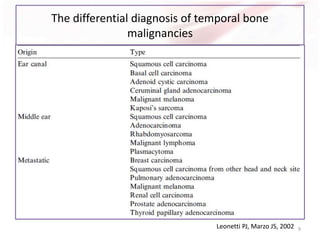
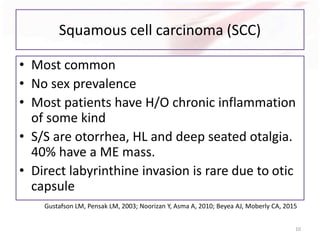
1) Temporal bone carcinoma is a rare and aggressive cancer, with squamous cell carcinoma being the most common type. It spreads along pathways in the temporal bone.
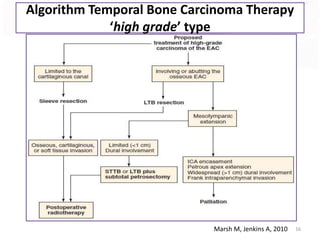
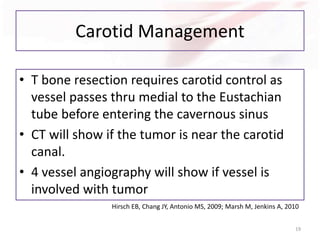
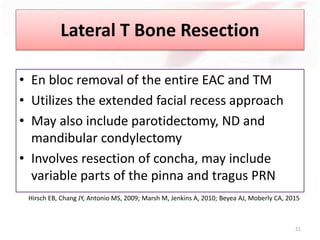
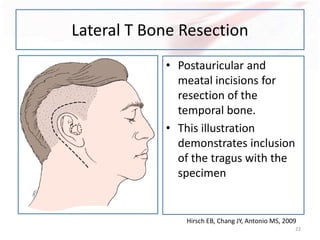
2) Surgery involves lateral, subtotal, or total temporal bone resection depending on tumor extent. More extensive resection provides wider margins but risks damage to nearby structures like cranial nerves.
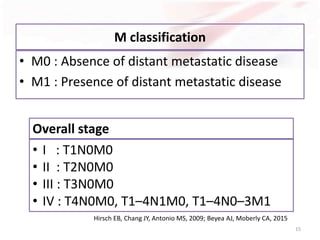
3) Prognosis depends on tumor stage - early T1/T2 stages have close to 100% 2-year survival while advanced T4 has only 17% 2-year survival, as these tumors have often spread beyond the temporal bone.